Melphalan 2mg Tablets
Melphalan
Melphalan 2mg Tablets
Melphalan is supplied as white, film-coated, round, biconvex tablets containing 2 mg melphalan in amber glass bottles with child-resistant closures. One side is engraved with “GX EH3” and the other side is engraved with an “A.”
Bottle of 50
Store in a refrigerator, 2° to 8°C (36° to 46°F). Protect from light.
Melphalan Tablets are indicated for the palliative treatment of multiple myeloma and for the palliation of non-resectable epithelial carcinoma of the ovary.
Melphalan is available in tablet form for oral administration. Each film-coated tablet contains 2 mg melphalan and the inactive ingredients colloidal silicon dioxide, crospovidone, hypromellose, macrogol/PEG 400, magnesium stearate, microcrystalline cellulose, and titanium dioxide.
Melphalan
Melphalan 2mg Tablets
What Melphalan is and what it is used for
The tablets contain a medicine called melphalan. This belongs to a group of medicines
called cytotoxics (also called chemotherapy). Melphalan is used to treat cancer. It works by
reducing the number of abnormal cells your body makes.
Melphalan is used for:
- Multiple myeloma – a type of cancer that develops from cells in the bone marrow called plasma cells. Plasma cells help to fight infection and disease by producing antibodies
- Advanced cancer of the ovaries
- Advanced breast cancer
- Polycythaemia vera – a disease which increases the number of red cells in your blood.
This makes the blood thicken and causes blood clots. This leads to headaches, dizziness and shortness of breath
Ask your doctor if you would like more explanation about these diseases.
Before you take Melphalan
Do not take Melphalan if:
- You are allergic (hypersensitive) to melphalan or any of the other ingredients of Melphalan tablets (See section 6: Further information)
- Do not take if any of the above apply to you. If you are not sure, talk to your doctor or pharmacist before taking Melphalan.
Take special care with Melphalan
Before you take Melphalan, tell your doctor or pharmacist if:
- You have had radiotherapy or chemotherapy, now or recently
- You have a kidney problem.
If you are not sure if any of the above apply to you, talk to your doctor or pharmacist before taking Melphalan.
Taking other medicines
Please tell your doctor or pharmacist if you are taking or have recently taken any other medicines, including medicines obtained without a prescription. This includes herbal medicines.
In particular, you must tell your doctor if you are taking any of the following:
- other cytotoxic drugs (chemotherapy)
- nalidixic acid (an antibiotic used to treat urinary tract infections)
- ciclosporin (used to prevent rejection of organs or tissues following a transplant or to treat certain skin conditions like psoriasis and eczema or to treat rheumatoid arthritis).
Having vaccines while you are taking Melphalan
If you are going to have a vaccination speak to your doctor or nurse before you have it. This is because some vaccines (like polio, measles, mumps and rubella) may give you an infection if you have them whilst you are taking Melphalan.
Pregnancy and breast-feeding
Do not take Melphalan if you are planning to have a baby. This applies to both men and women. Melphalan may harm your sperm or eggs. Reliable contraceptive precautions must be taken to avoid pregnancy whilst you or your partner are taking these tablets. Ask your doctor for advice. If you are already pregnant, it is important to talk to your doctor before taking Melphalan. Do not breast-feed while taking Melphalan. Ask your doctor or midwife for advice.
How to take Melphalan
Melphalan should only be given to you by a specialist doctor who is experienced in treating blood problems or cancer. Always take Melphalan exactly as your doctor has told you. It is important to take your medicine at the right times. The label on your pack will tell you how many tablets to take and how often to take them. If the label doesn’t say or if you are not sure, ask your doctor, nurse or pharmacist.
- Swallow your tablets whole with a glass of water.
Do not break, crush or chew the tablets.
The dose of Melphalan depends on your blood problem or cancer (see section 1).
- Your doctor may also change your dose during your treatment, depending on your needs.
- The dose can sometimes be changed if you are elderly or have a kidney problem.
- When you take Melphalan, your doctor will take regular blood tests. This is to check the number of cells in your blood. Your doctor may sometimes change your dose as a result.
Multiple myeloma
- The usual dose is 0.15mg per kilogram of your body weight each day for 4 days.
This is repeated every 6 weeks.
Advanced ovarian adenocarcinoma
- The usual dose is 0.2mg per kilogram of your body weight each day for 5 days.
This is repeated every 4 to 8 weeks.
Advanced breast carcinoma
- The usual dose is 0.15mg per kilogram of your body weight each day for 5 days.
This is repeated every 6 weeks.
Polycythaemia vera
- Initially 6 to 10mg each day for 5 to 7 days. The dose will then be reduced to 2 to 4mg each day.
If you take more Melphalan than you should
- If you take more Melphalan than you should, tell your doctor immediately or go to a hospital straight away. Take the medicine pack with you.
If you forget to take Melphalan
Tell your doctor. Do not take a double dose to make up for a forgotten dose.
Possible side effects
Like all medicines, Melphalan can cause side effects, although not everybody gets them.
If you get any of the following, talk to your specialist doctor or go to hospital straight away:
- allergic reaction, the signs may include:
- a rash, lumps or hives on the skin
- swollen face, eyelids or lips
- sudden wheeziness and tightness of the chest
- collapse (due to cardiac arrest)
- any signs of fever or infection (sore throat, sore mouth or urinary problems)
- any unexpected bruising or bleeding or feeling extremely tired, dizzy or breathless, as this could mean that too few blood cells of a particular type are being produced
- if you suddenly feel unwell (even with a normal temperature).
Talk to your doctor if you have any of the following side effects which may also happen with this medicine:
Very common (affects more than 1 in 10 people)
- a drop in the number of blood cells and platelets
- feeling sick (nausea), being sick (vomiting) and diarrhoea
- mouth ulcers - with high doses of Melphalan
- hair loss - with high doses of Melphalan
Common (affects less than 1 in 10 people)
- hair loss - with usual doses of Melphalan
- high levels of a chemical called urea in your blood – in people with kidney problems who are being treated for myeloma
Rare (affects less than 1 in 1,000 people)
- an illness where you have a low number of red blood cells as they are being destroyed prematurely – this can make you feel very tired, breathless and dizzy and can give you headaches or make your skin or eyes yellow
- lung problems which may make you cough or wheeze and make it difficult to breathe
- liver problems which may show up in your blood tests or cause jaundice (yellowing of the whites of eyes and skin)
- mouth ulcers – with normal doses of Melphalan
- skin rashes or itching skin
The following side effects also happen with Melphalan:
- leukaemia – cancer of the blood
- in women: your periods stopping
If any of the side effects gets serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist.
How to store Melphalan
- Keep out of the reach and sight of children.
- Do not use Melphalan after the expiry date which is stated on the pack after ‘Exp’.
- Store in a refrigerator between 2 and 8°C.
- If your doctor tells you to stop taking the tablets, it is important to return any which are left over to your pharmacist, who will destroy them according to disposal of dangerous substance guidelines. Only keep the tablets if your doctor tells you to.
Further information
What Melphalan contains
The active ingredient is melphalan.
Each Melphalan tablet contains 2mg of melphalan.
The other ingredients are:
- microcrystalline cellulose,
- crospovidone,
- colloidal anhydrous silica,
- magnesium stearate,
- hypromellose,
- titanium dioxide and
- macrogol.
What Melphalan looks like and contents of the pack
Melphalan tablets are white to off-white film-coated, round, biconvex tablets engraved with ‘T’ on one side and ‘2’ on the other.
Melphalan tablets are in bottles of 25 tablets.
Melphalan
Melphalan 2mg Tablets
DESCRIPTION
Melphalan, also known as L-phenylalanine mustard, phenylalanine mustard, L-PAM, or L-sarcolysin, is a phenylalanine derivative of nitrogen mustard. Melphalan is a bifunctional alkylating agent which is active against selective human neoplastic diseases. It is known chemically as 4-[bis(2-chloroethyl)amino]-L-phenylalanine. The molecular formula is C13H18Cl2N2O2 and the molecular weight is 305.20. The structural formula is:

Melphalan is the active L-isomer of the compound and was first synthesized in 1953 by Bergel and Stock; the D-isomer, known as medphalan, is less active against certain animal tumors, and the dose needed to produce effects on chromosomes is larger than that required with the L-isomer. The racemic (DL-) form is known as merphalan or sarcolysin.
Melphalan is practically insoluble in water and has a pKa1 of ~2.5.
Melphalan (melphalan) is available in tablet form for oral administration. Each film-coated tablet contains 2 mg melphalan and the inactive ingredients colloidal silicon dioxide, crospovidone, hypromellose, macrogol/PEG 400, magnesium stearate, microcrystalline cellulose, and titanium dioxide.
CLINICAL PHARMACOLOGY
Melphalan is an alkylating agent of the bischloroethylamine type. As a result, its cytotoxicity appears to be related to the extent of its interstrand cross-linking with DNA, probably by binding at the N7 position of guanine. Like other bifunctional alkylating agents, it is active against both resting and rapidly dividing tumor cells.
Pharmacokinetics
The absorption of oral melphalan is highly variable with respect to both the time to first appearance of the drug in plasma (range: 0 to 6 hours) and peak plasma concentration (Cmax). The average absolute bioavailability of melphalan is also highly variable (range: 56% to 93%). These results may be due to incomplete intestinal absorption, a variable “first pass” hepatic metabolism, or to rapid hydrolysis. Oral administration of melphalan with a high fat meal may reduce melphalan exposure (AUC) by 36% to 54%.
In 18 patients given a single oral dose of 0.6 mg/kg of Melphalan, the terminal elimination plasma half-life (t1/2) of parent drug was 1.5 ± 0.83 hours. The 24-hour urinary excretion of parent drug in these patients was 10% ± 4.5%, suggesting that renal clearance is not a major route of elimination of parent drug. In a separate study in 18 patients given single oral doses of 0.2 to 0.25 mg/kg of Melphalan, Cmax and plasma concentration-time curves (AUC), when dose adjusted to a dose of 14 mg, were (mean ± SD) 212 ± 74 ng/mL and 498 ± 137 ng•hr/mL, respectively. Elimination phase t½ in these patients was approximately 1 hour and the median tmax was 1 hour.
One study using universally labeled 14C-melphalan, found substantially less radioactivity in the urine of patients given the drug by mouth (30% of administered dose in 9 days) than in the urine of those given it intravenously (35% to 65% in 7 days). Following either oral or IV administration, the pattern of label recovery was similar, with the majority being recovered in the first 24 hours. Following oral administration, peak radioactivity occurred in plasma at 2 hours and then disappeared with a half-life of approximately 160 hours. In 1 patient where parent drug (rather than just radiolabel) was determined, the melphalan half-disappearance time was 67 minutes.
The steady-state volume of distribution of melphalan is 0.5 L/kg. Penetration into cerebrospinal fluid (CSF) is low. The average melphalan binding to plasma proteins is highly variable (range: 53% to 92%). Serum albumin is the major binding protein, accounting for approximately 40% to 60% of the plasma protein binding, while a1-acid glycoprotein accounts for about 20% of the plasma protein binding. Approximately 30% of melphalan is (covalently) irreversibly bound to plasma proteins. Interactions with immunoglobulins have been found to be negligible.
Melphalan is eliminated from plasma primarily by chemical hydrolysis to monohydroxymelphalan and dihydroxymelphalan. Aside from these hydrolysis products, no other melphalan metabolites have been observed in humans. Although the contribution of renal elimination to melphalan clearance appears to be low, one pharmacokinetic study showed a significant positive correlation between the elimination rate constant for melphalan and renal function and a significant negative correlation between renal function and the area under the plasma melphalan concentration/time curve.
INDICATIONS AND USAGE
Melphalan Tablets are indicated for the palliative treatment of multiple myeloma and for the palliation of non-resectable epithelial carcinoma of the ovary.
CONTRAINDICATIONS
Melphalan should not be used in patients whose disease has demonstrated a prior resistance to this agent. Patients who have demonstrated hypersensitivity to melphalan should not be given the drug.
WARNINGS
Melphalan should be administered in carefully adjusted dosage by or under the supervision of experienced physicians who are familiar with the drug's actions and the possible complications of its use.
As with other nitrogen mustard drugs, excessive dosage will produce marked bone marrow suppression. Bone marrow suppression is the most significant toxicity associated with Melphalan in most patients. Therefore, the following tests should be performed at the start of therapy and prior to each subsequent course of Melphalan: platelet count, hemoglobin, white blood cell count, and differential. Thrombocytopenia and/or leukopenia are indications to withhold further therapy until the blood counts have sufficiently recovered. Frequent blood counts are essential to determine optimal dosage and to avoid toxicity (see PRECAUTIONS: Laboratory Tests). Dose adjustment on the basis of blood counts at the nadir and day of treatment should be considered.
Hypersensitivity reactions, including anaphylaxis, have occurred rarely (see ADVERSE REACTIONS). These reactions have occurred after multiple courses of treatment and have recurred in patients who experienced a hypersensitivity reaction to IV Melphalan. If a hypersensitivity reaction occurs, oral or IV Melphalan should not be readministered.
Carcinogenesis
Secondary malignancies, including acute nonlymphocytic leukemia, myeloproliferative syndrome, and carcinoma have been reported in patients with cancer treated with alkylating agents (including melphalan). Some patients also received other chemotherapeutic agents or radiation therapy. Precise quantitation of the risk of acute leukemia, myeloproliferative syndrome, or carcinoma is not possible. Published reports of leukemia in patients who have received melphalan (and other alkylating agents) suggest that the risk of leukemogenesis increases with chronicity of treatment and with cumulative dose. In one study, the 10-year cumulative risk of developing acute leukemia or myeloproliferative syndrome after melphalan therapy was 19.5% for cumulative doses ranging from 730 mg to 9,652 mg. In this same study, as well as in an additional study, the 10-year cumulative risk of developing acute leukemia or myeloproliferative syndrome after melphalan therapy was less than 2% for cumulative doses under 600 mg. This does not mean that there is a cumulative dose below which there is no risk of the induction of secondary malignancy. The potential benefits from melphalan therapy must be weighed on an individual basis against the possible risk of the induction of a second malignancy.
Adequate and well-controlled carcinogenicity studies have not been conducted in animals. However, i.p. administration of melphalan in rats (5.4 to 10.8 mg/m2) and in mice (2.25 to 4.5 mg/m2) 3 times per week for 6 months followed by 12 months post-dose observation produced peritoneal sarcoma and lung tumors, respectively.
Mutagenesis
Melphalan has been shown to cause chromatid or chromosome damage in humans. Intramuscular administration of Melphalan at 6 and 60 mg/m2 produced structural aberrations of the chromatid and chromosomes in bone marrow cells of Wistar rats.
Impairment of Fertility
Melphalan causes suppression of ovarian function in premenopausal women, resulting in amenorrhea in a significant number of patients. Reversible and irreversible testicular suppression have also been reported.
Pregnancy
Pregnancy Category D.
Melphalan may cause fetal harm when administered to a pregnant woman. Melphalan was embryolethal and teratogenic in rats following oral (6 to 18 mg/m2/day for 10 days) and intraperitoneal (18 mg/m2) administration. Malformations resulting from melphalan included alterations of the brain (underdevelopment, deformation, meningocele, and encephalocele) and eye (anophthalmia and microphthalmos), reduction of the mandible and tail, as well as hepatocele (exomphaly).
There are no adequate and well-controlled studies in pregnant women. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus. Women of childbearing potential should be advised to avoid becoming pregnant.
PRECAUTIONS
General
In all instances where the use of Melphalan is considered for chemotherapy, the physician must evaluate the need and usefulness of the drug against the risk of adverse events. Melphalan should be used with extreme caution in patients whose bone marrow reserve may have been compromised by prior irradiation or chemotherapy, or whose marrow function is recovering from previous cytotoxic therapy. If the leukocyte count falls below 3,000 cells/mcL, or the platelet count below 100,000 cells/mcL, Melphalan should be discontinued until the peripheral blood cell counts have recovered.
A recommendation as to whether or not dosage reduction should be made routinely in patients with renal insufficiency cannot be made because:
a) There is considerable inherent patient-to-patient variability in the systemic availability of melphalan in patients with normal renal function.
b) Only a small amount of the administered dose appears as parent drug in the urine of patients with normal renal function.
Patients with azotemia should be closely observed, however, in order to make dosage reductions, if required, at the earliest possible time.
Administration of live vaccines to immunocompromised patients should be avoided.
Information for Patients
Patients should be informed that the major toxicities of Melphalan are related to bone marrow suppression, hypersensitivity reactions, gastrointestinal toxicity, and pulmonary toxicity. The major long-term toxicities are related to infertility and secondary malignancies. Patients should never be allowed to take the drug without close medical supervision and should be advised to consult their physician if they experience skin rash, vasculitis, bleeding, fever, persistent cough, nausea, vomiting, amenorrhea, weight loss, or unusual lumps/masses. Women of childbearing potential should be advised to avoid becoming pregnant.
Laboratory Tests
Periodic complete blood counts with differentials should be performed during the course of treatment with Melphalan. At least one determination should be obtained prior to each treatment course. Patients should be observed closely for consequences of bone marrow suppression, which include severe infections, bleeding, and symptomatic anemia (see WARNINGS).
Drug Interactions
There are no known drug/drug interactions with oral Melphalan.
Carcinogenesis, Mutagenesis, Impairment of Fertility
See WARNINGS section.
Pregnancy
Teratogenic Effects
Pregnancy Category D: See WARNINGS section.
Nursing Mothers
It is not known whether this drug is excreted in human milk. Melphalan should not be given to nursing mothers.
Pediatric Use
The safety and effectiveness of Melphalan in pediatric patients have not been established.
Geriatric Use
Clinical studies of Melphalan Tablets did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
ADVERSE REACTIONS
Hematologic
The most common side effect is bone marrow suppression leading to leukopenia, thrombocytopenia, and anemia. Although bone marrow suppression frequently occurs, it is usually reversible if melphalan is withdrawn early enough. However, irreversible bone marrow failure has been reported.
Gastrointestinal
Nausea, vomiting, diarrhea, and oral ulceration occur. Hepatic disorders ranging from abnormal liver function tests to clinical manifestations such as hepatitis and jaundice have been reported.
Miscellaneous
Other reported adverse reactions include: pulmonary fibrosis (including fatal outcomes) and interstitial pneumonitis, skin hypersensitivity, maculopapular rashes, vasculitis, alopecia, and hemolytic anemia. Allergic reactions, including urticaria, edema, skin rashes, and rare anaphylaxis, have occurred after multiple courses of treatment. Cardiac arrest has also been reported rarely in association with such reports.
OVERDOSAGE
Overdoses, including doses up to 50 mg/day for 16 days, have been reported. Immediate effects are likely to be vomiting, ulceration of the mouth, diarrhea, and hemorrhage of the gastrointestinal tract. The principal toxic effect is bone marrow suppression. Hematologic parameters should be closely followed for 3 to 6 weeks. An uncontrolled study suggests that administration of autologous bone marrow or hematopoietic growth factors (i.e., sargramostim, filgrastim) may shorten the period of pancytopenia. General supportive measures, together with appropriate blood transfusions and antibiotics, should be instituted as deemed necessary by the physician. This drug is not removed from plasma to any significant degree by hemodialysis.
DOSAGE AND ADMINISTRATION
Multiple Myeloma
The usual oral dose is 6 mg (3 tablets) daily. The entire daily dose may be given at one time. The dose is adjusted, as required, on the basis of blood counts done at approximately weekly intervals. After 2 to 3 weeks of treatment, the drug should be discontinued for up to 4 weeks, during which time the blood count should be followed carefully. When the white blood cell and platelet counts are rising, a maintenance dose of 2 mg daily may be instituted. Because of the patient-to-patient variation in melphalan plasma levels following oral administration of the drug, several investigators have recommended that the dosage of Melphalan be cautiously escalated until some myelosuppression is observed in order to assure that potentially therapeutic levels of the drug have been reached.
Other dosage regimens have been used by various investigators. Osserman and Takatsuki have used an initial course of 10 mg/day for 7 to 10 days. They report that maximal suppression of the leukocyte and platelet counts occurs within 3 to 5 weeks and recovery within 4 to 8 weeks. Continuous maintenance therapy with 2 mg/day is instituted when the white blood cell count is greater than 4,000 cells/mcL and the platelet count is greater than 100,000 cells/mcL. Dosage is adjusted to between 1 and 3 mg/day depending upon the hematological response. It is desirable to try to maintain a significant degree of bone marrow depression so as to keep the leukocyte count in the range of 3,000 to 3,500 cells/mcL.
Hoogstraten et al have started treatment with 0.15 mg/kg/day for 7 days. This is followed by a rest period of at least 14 days, but it may be as long as 5 to 6 weeks. Maintenance therapy is started when the white blood cell and platelet counts are rising. The maintenance dose is 0.05 mg/kg/day or less and is adjusted according to the blood count.
Available evidence suggests that about one third to one half of the patients with multiple myeloma show a favorable response to oral administration of the drug.
One study by Alexanian et al has shown that the use of Melphalan in combination with prednisone significantly improves the percentage of patients with multiple myeloma who achieve palliation. One regimen has been to administer courses of Melphalan at 0.25 mg/kg/day for 4 consecutive days (or, 0.20 mg/kg/day for 5 consecutive days) for a total dose of 1 mg/kg/course. These 4- to 5-day courses are then repeated every 4 to 6 weeks if the granulocyte count and the platelet count have returned to normal levels.
It is to be emphasized that response may be very gradual over many months; it is important that repeated courses or continuous therapy be given since improvement may continue slowly over many months, and the maximum benefit may be missed if treatment is abandoned too soon.
In patients with moderate to severe renal impairment, currently available pharmacokinetic data do not justify an absolute recommendation on dosage reduction to those patients, but it may be prudent to use a reduced dose initially.
Epithelial Ovarian Cancer
One commonly employed regimen for the treatment of ovarian carcinoma has been to administer Melphalan at a dose of 0.2 mg/kg daily for 5 days as a single course. Courses are repeated every 4 to 5 weeks depending upon hematologic tolerance.
Administration Precautions
Procedures for proper handling and disposal of anticancer drugs should be considered. Several guidelines on this subject have been published.1-4
There is no general agreement that all of the procedures recommended in the guidelines are necessary or appropriate.
HOW SUPPLIED
Melphalan is supplied as white, film-coated, round, biconvex tablets containing 2 mg melphalan in amber glass bottles with child-resistant closures. One side is engraved with “GX EH3” and the other side is engraved with an “A.”
Bottle of 50.
Store in a refrigerator, 2° to 8°C (36° to 46°F). Protect from light.
REFERENCES
- 1.
- NIOSH Alert: Preventing Occupational Exposures to Antineoplastic and Other Hazardous Drugs in Healthcare Settings. U.S. Department of Health and Human Services, Public Health Service. Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 2004-165.
- 2.
- OSHA Technical Manual, TED 1-0.15A, Section VI: Chapter 2. Controlling Occupational Exposure to Hazardous Drugs. OSHA, 1999. http://www.osha.gov/dts/osta/otm/otm_vi/otm_vi_2.html
- 3.
- American Society of Health-System Pharmacists. (2006) ASHP Guidelines on Handling Hazardous Drugs. Am J Health-Syst Pharm. 2006;63:1172-1193.
- 4.
- Polovich M, White JM, Kelleher LO (eds.) 2005. Chemotherapy and Biotherapy Guidelines and Recommendations for Practice. (2nd ed.) Pittsburgh, PA: Oncology Nursing Society.
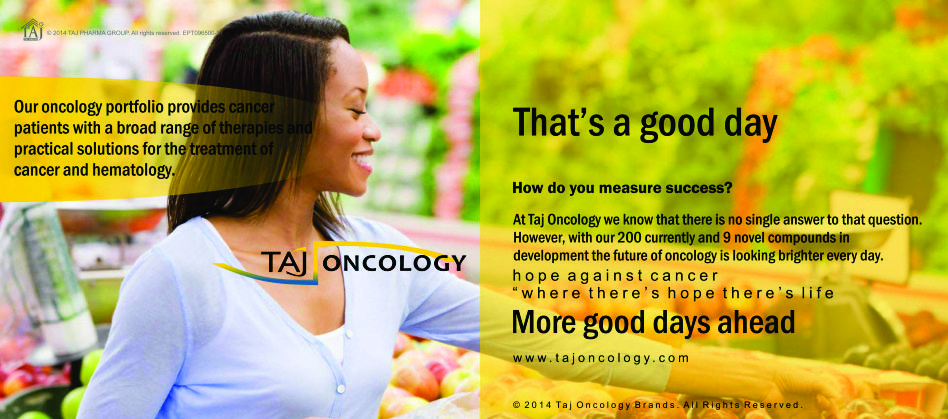
Product Glimpse
Description
We are committed to work towards a healthier and happier world. The company is an integrated, research based international pharmaceutical company, producing a wide range of quality, affordable generic (Melphalan 2mg/5mg Tablets) medicines, trusted by health-care professionals and patients across geographies.
We offer you the highest quality new Generic medicines ie. Melphalan 2mg/5mg Tablets, drugs and also with innovative packing at the lowest prices shipped to you from India. Browse our latest Pharmaceuticals and Generics possibilities and other pharmaceuticals possibilities…more.