Lomustine 10mg/40mg/100mg Capsules
Lomustine
Lomustine 10mg/40mg/100mg Capsules
Lomustine Capsules are available in individual bottles of 5 capsules each.
100 mg capsules (Green/Green)
40 mg capsules (White/Green)
10 mg capsules (White/White)
Stability
Lomustine Capsules are stable for the lot life indicated on package labeling when stored in well-closed containers at 25°C (77°F); excursions permitted to 15°C–30°C (59°F–86°F) [see USP Controlled Room Temperature]. Avoid excessive heat (over 40°C, 104°F).
Lomustine (CCNU) is one of the nitrosoureas used in the treatment of certain neoplastic diseases. It is 1-(2-chloro-ethyl)-3-cyclohexyl-1-nitrosourea. It is a yellow powder with the empirical formula of C9H16ClN3O2 and a molecular weight of 233.71. Lomustine is soluble in 10% ethanol (0.05 mg per mL) and in absolute alcohol (70 mg per mL). Lomustine is relatively insoluble in water (<0.05 mg per mL).
It is relatively un-ionized at a physiological pH.
Inactive ingredients in Lomustine Capsules are magnesium stearate and mannitol.
Taj Oncology Generics
WHAT LOMUSTINE IS AND WHAT IT IS USED FOR
This medicine contains an active ingredient called lomustine.
Lomustine belongs to a group of medicines called antineoplastic or cytotoxic agents. These medicines affect growth and proliferation of cancer cells.
Lomustine capsules are used to treat tumours and other malignant growths or diseases, for example, cancer of the lung or skin.
BEFORE YOU TAKE LOMUSTINE
Do not take Lomustine if you
- are allergic (hypersensitive) to lomustine or any of the other ingredients of Lomustine .
- have had a similar medicine before which you had to stop taking because of side effects or because it was ineffective.
- have any blood disorder.
- have severe kidney problems.
- have coeliac disease (your body cannot digest gluten) or wheat allergy.
- have had a vaccination against yellow fever or another live vaccine vaccination and suffer from immunosuppression.
- are pregnant or breastfeeding.
You and your partner should avoid contraception (becoming pregnant or fathering children) during treatment and for at least 6 months after your treatment with lomustine has stopped.
Take special care with Lomustine
- Do not take a higher dose of lomustine as prescribed by your doctor and do not repeat treatment before the end of 6 weeks.
- Your doctor will check your blood weekly during your therapy and up to 6 weeks afterwards.
- Lomustine might impair the function of your blood-building system, and increase the risk of bleeding and infections. This effect might occur after a certain time of therapy.
- As the toxic effects of lomustine to your blood-building system are cumulative your doctor might decide to adjust the dosage of your therapy.
- Tell your doctor if you have any liver problems. Before you start with lomustine, your doctor will check the function of your liver and additionally of your lung and kidney. These tests will be repeated during the time of your therapy.
- Long term use of nitrosoureas has been reported to be possibly associated with the development of secondary malignancies.
Taking other medicines
No special studies regarding interactions between lomustine and other drugs have been performed, but tell your doctor if you are taking any of the following medicines:
- theophylline – medicine used in the treatment of respiratory tract diseases, e.g. asthma
- cimetidine – medicine largely used in the treatment of heartburn and peptic ulcers
- other chemotherapeutic drugs, because co-administration can lead to complications secondary to pharmacokinetic interactions between the drugs.
Tell your doctor if you have ever taken phenobarbital – an anticonvulsant or another antiepileptic drug.
You should also inform your doctor if you recently have been vaccinated.
Please tell your doctor or pharmacist if you are taking or have recently taken any other medicines, including medicines obtained without a prescription.
Fertility, pregnancy and breastfeeding
Ask your doctor or pharmacist for advice before taking any medicine.
Pregnancy
Pregnant women should not receive this medicine. It is important to tell your doctor if you are pregnant or think you might be pregnant, because safe use in pregnancy has not been established. If you become
pregnant while you are treated with lomustine tell your doctor immediately, as taking lomustine might affect your unborn baby detrimentally. If you are in the childbearing age you should avoid becoming pregnant.
Breast-feeding
You should not breast-feed your baby while being treated with this medicine, because lomustine might be excreted in your breast milk. As a risk to the nursing child potentially exists, a decision should be made whether to discontinue breast-feeding or to discontinue lomustine therapy taking into account the benefit of breast-feeding for the child and the benefit of therapy for the mother.
Fertility
Men who are treated with lomustine should not father a child during their therapy and up to 6 month afterwards. As lomustine may affect your fertility, ask your doctor to inform you about possible precautions like sperm conservation before you start with the treatment.
Driving and using machines
No special studies have been performed, but Lomustine capsules can impair your ability to drive and use machines, e.g. because of nausea and vomiting.
Important information about some of the ingredients of Lomustine
This medicinal product contains lactose. If you have been told by your doctor that you have an intolerance to some sugars, contact your doctor before taking this medicinal product.
This medicinal product also contains wheat starch. Patients with wheat allergy or coeliac disease should not take this medicine (see above “Do not take Lomustine”).
HOW TO TAKE LOMUSTINE
Care must be taken whenever handling anticancer products. Caution! Do not break open the Lomustine capsules. If you accidentally get the powder on your skin or in your mouth, wash it off with plenty of water. Wash your hands with soap and water after handling this product.
Always take Lomustine exactly as your doctor has told you, and in an interval not less than 6 weeks. You should check with your doctor or pharmacist if you are not sure.
Lomustine capsules are taken by mouth. Swallow the capsules whole, do not chew or break them.
Adults
Your doctor will decide the exact dose to give you and how often to give it. Usually the dose depends on your height and weight. You may expect to receive 200 – 240 mg lomustine. Lomustine capsules are usually taken once every 6 to 8 weeks either as a single dose or as a divided dose over 3 days, e.g. 80 mg/day.
The dose you take may be reduced if you are taking other drugs to treat your condition or if you have a blood disorder.
Children
Lomustine capsules may be used in children with certain types of tumour. You must only use Lomustine for children as prescribed by the doctor.
Lomustine capsules are usually taken once every 6 to 8 weeks either as a single dose or as a divided dose over 3 days, e.g. 40 mg/day.
If you take more Lomustine than you should Accidental overdose with lomustine has been reported, including fatal cases.
If you have taken too much medication please consult your doctor or local casualty department immediately.
An overdose might express in abdominal pain, diarrhea, regurgitation, lack of appetite, lethargy, a feeling of dizziness, cough or shortness of breath.
If you forget to take Lomustine
It is important to complete the course of medication exactly as prescribed by your doctor. If you think you have missed a dose for any reason please tell your doctor or nurse immediately. Your doctor will decide how to proceed with the intake of Lomustine. If you have any further questions on the use of this product, ask your doctor or pharmacist.
POSSIBLE SIDE EFFECTS
Like all medicines, Lomustine can cause side effects, although not everybody gets them.
The unwanted effects could include:
Gastrointestinal disorders
- Nausea and vomiting usually occur about 3 – 6 hours after taking a full single dose and lasts for 24 – 48 hours. This is followed by 2 – 3 days loss of appetite. Your doctor may prescribe another type of medicine (antiemetics) for you to take at the same time to help with these side effects. Nausea, vomiting and loss of appetite may be less troublesome if you take Lomustine capsules as a divided dose over 3 days. It might also help to take lomustine on an empty stomach.
- Stomatitis (inflammation inside the mouth) and diarrhoea have occurred rarely.
Blood and liver disorders
- If you are affected by blood and liver disorders you may, for example, find you bruise more easily, or you may repeatedly get infections such as sore throat or cough. If this occurs report immediately to your doctor. Your doctor will probably carry out regular blood tests while you are on Lomustine capsules therapy to monitor these side effects.
- Lomustine may produce cumulative myelosuppression, manifested by more depressed indices or longer duration of suppression after repeated doses.
- Acute leukaemia (blood cancer), and myelodysplastic syndrome (blood-related medical conditions that involve ineffective production of the myeloid class of blood cells) have been reported in patients following long term nitrosurea therapy, but frequency cannot be estimated from the available data.
- A reversible type of liver toxicity, manifested by increased liver parameters (transaminases, alkaline phosphatase, and bilirubin levels), has been reported in a small percentage of patients receiving lomustine.
Nervous system disorders
- Mild neurological symptoms, like lack of interest (apathy), lethargy, disorientation, abnormal coordination, confusion and stuttering or speech defects can occur.
Lung disorders
- Pneumonia has occurred rarely.
- Lung fibrosis (formation of binding tissue in the lungs) and lung infiltration (accumulation of substances or fluid in the lung) might occur; frequency not known.
- Pulmonary toxicity has been described to occur after an interval of 6 months or longer from the start of therapy with high total doses (> than 1,100 mg/m²). There is one report of pulmonary toxicity with a total dose of 600 mg.
- Delayed onset of pulmonary fibrosis occurring up to 17 years after treatment has been reported in patients with intracranial tumors who received related nitrosoureas during their childhood and early adolescence.
Skin disorders
- Loss of hair has been reported infrequently. Kidney disorders
- Kidney disorders have occurred in single cases.
- Failure of the kidney, azotaemia (increase of nitrogenous compounds in your blood) and decrease in kidney size after prolonged treatment and large total dose has been reported for lomustine and related nitrosoureas. Kidney damage has also been reported occasionally in patients receiving lower total doses.
Eye disorders
- After combined therapy with radiation an irreversible vision loss has been reported in single cases.
If any of the side effects gets serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist.
HOW TO STORE LOMUSTINE
Keep out of the reach and sight of children.
Do not store above 25 °C.
Keep the box in the outer carton in order to protect from light and moisture.
Do not use Lomustine after the expiry date which is stated on the box. The expiry date refers to the last day of that month.
At the end of treatment return any leftover medicine to your hospital or pharmacist.
FURTHER INFORMATION
What Lomustine contains
The active substance is lomustine. Each capsule contains 40 mg lomustine.
The other ingredients are lactose, wheat starch, talc and magnesium stearate.
The capsule is made of gelatin and the colouring agents titanium dioxide (E171) and indigotine (E132).
What Lomustine looks like and contents of the pack
Lomustine are blue hard capsules. Lomustine capsules are packed in a plastic box. There are 20 capsules in each pack.
Taj Oncology generics
DESCRIPTION
Lomustine (CCNU) is one of the nitrosoureas used in the treatment of certain neoplastic diseases. It is 1-(2-chloro-ethyl)-3-cyclohexyl-1-nitrosourea. It is a yellow powder with the empirical formula of C9H16ClN3O2 and a molecular weight of 233.71. Lomustine is soluble in 10% ethanol (0.05 mg per mL) and in absolute alcohol (70 mg per mL). Lomustine is relatively insoluble in water (<0.05 mg per mL).
It is relatively un-ionized at a physiological pH.
Inactive ingredients in Lomustine Capsules are magnesium stearate and mannitol.
The structural formula is:

Lomustine is available in 10 mg, 40 mg, and 100 mg capsules for oral administration.
CLINICAL PHARMACOLOGY
Although it is generally agreed that lomustine alkylates DNA and RNA, it is not cross resistant with other alkylators. As with other nitrosoureas, it may also inhibit several key enzymatic processes by carbamoylation of amino acids in proteins.
Lomustine may be given orally. Following oral administration of radioactive lomustine at doses ranging from 30 mg/m2 to 100 mg/m2, about half of the radioactivity given was excreted in the urine in the form of degradation products within 24 hours.
The serum half-life of the metabolites ranges from 16 hours to 2 days. Tissue levels are comparable to plasma levels at 15 minutes after intravenous administration.
Because of the high lipid solubility and the relative lack of ionization at physiological pH, lomustine crosses the blood-brain barrier quite effectively. Levels of radioactivity in the CSF are 50% or greater than those measured concurrently in plasma.
INDICATIONS AND USAGE
Lomustine has been shown to be useful as a single agent in addition to other treatment modalities, or in established combination therapy with other approved chemotherapeutic agents in the following:
Brain tumors
—both primary and metastatic, in patients who have already received appropriate surgical and/or radiotherapeutic procedures.
Hodgkin's disease
—secondary therapy in combination with other approved drugs in patients who relapse while being treated with primary therapy, or who fail to respond to primary therapy.
CONTRAINDICATIONS
Lomustine should not be given to individuals who have demonstrated a previous hypersensitivity to it.
WARNINGS
Since the major toxicity is delayed bone marrow suppression, blood counts should be monitored weekly for at least 6 weeks after a dose (see ADVERSE REACTIONS). At the recommended dosage, courses of Lomustine should not be given more frequently than every 6 weeks.
The bone marrow toxicity of Lomustine is cumulative and therefore dosage adjustment must be considered on the basis of nadir blood counts from prior dose (see dosage adjustment table under DOSAGE AND ADMINISTRATION).
Pulmonary toxicity from Lomustine appears to be dose related (see ADVERSE REACTIONS).
Long-term use of nitrosoureas has been reported to be possibly associated with the development of secondary malignancies.
Liver and renal function tests should be monitored periodically (see ADVERSE REACTIONS).
Pregnancy Category D
Lomustine can cause fetal harm when administered to a pregnant woman. Lomustine is embryotoxic and teratogenic in rats and embryotoxic in rabbits at dose levels equivalent to the human dose. There are no adequate and well controlled studies in pregnant women. If this drug is used during pregnancy, or if the patient becomes pregnant while taking (receiving) this drug, the patient should be apprised of the potential hazard to the fetus. Women of childbearing potential should be advised to avoid becoming pregnant.
PRECAUTIONS
General
In all instances where the use of Lomustine is considered for chemotherapy, the physician must evaluate the need and usefulness of the drug against the risks of toxic effects or adverse reactions. Most such adverse reactions are reversible if detected early. When such effects or reactions do occur, the drug should be reduced in dosage or discontinued and appropriate corrective measures should be taken according to the clinical judgment of the physician. Reinstitution of Lomustine therapy should be carried out with caution and with adequate consideration of the further need for the drug and alertness as to possible recurrence of toxicity.
Information for Patients
Provide patients with the following information and instructions:
- In order to provide the proper dose of Lomustine, the dose may be made up of 2 or more different strengths and colors of capsules. Each strength must be dispensed separately by the pharmacist.
- Lomustine is given as a single oral dose and will not be repeated for at least 6 weeks. Daily use of the recommended dose may lead to toxicities and fatal outcomes.
- Patients may experience nausea and vomiting that usually last less than 24 hours. Patients may also experience loss of appetite that may last for several days.
- Instruct patients to contact their physician if they develop any of the following reactions: fever, chills, sore throat, unusual bleeding or bruising, shortness of breath, dry cough, swelling of feet or lower legs, mental confusion, or yellowing of eyes and skin.
- Instruct patients to wear impervious (rubber or latex) gloves when handling Lomustine Capsules.
Laboratory Tests
Due to delayed bone marrow suppression, blood counts should be monitored weekly for at least 6 weeks after a dose.
Baseline pulmonary function studies should be conducted along with frequent pulmonary function tests during treatment. Patients with a baseline below 70% of the predicted Forced Vital Capacity (FVC) or Carbon Monoxide Diffusing Capacity (DLCO) are particularly at risk.
Since Lomustine may cause liver dysfunction, it is recommended that liver function tests be monitored periodically.
Renal function tests should also be monitored periodically.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Lomustine is carcinogenic in rats and mice, producing a marked increase in tumor incidence in doses approximating those employed clinically. Nitrosourea therapy does have carcinogenic potential in humans. Lomustine also affects fertility in male rats at doses somewhat higher than the human dose.
Pregnancy
Pregnancy Category D See WARNINGS.
Nursing Mothers
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from Lomustine, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
See ADVERSE REACTIONS: Pulmonary Toxicity and DOSAGE AND ADMINISTRATION.
Geriatric Use
No data from clinical studies of Lomustine are available for patients 65 years of age and over to determine whether they respond differently than younger patients. Other reported clinical experience has not identified differences in responses between elderly and younger patients. In general, dose selection for an elderly patient should be cautious, reflecting the greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or other drug therapy.
Lomustine and its metabolites are known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and renal function should be monitored.
ADVERSE REACTIONS
Hematologic Toxicity
The most frequent and most serious toxicity of Lomustine is delayed myelosuppression. It usually occurs 4 to 6 weeks after drug administration and is dose related. Thrombocytopenia occurs at about 4 weeks postadministration and persists for 1 to 2 weeks. Leukopenia occurs at 5 to 6 weeks after a dose of Lomustine and persists for 1 to 2 weeks. Approximately 65% of patients receiving 130 mg/m2 develop white blood counts below 5000 wbc/mm3. Thirty-six percent developed white blood counts below 3000 wbc/mm3. Thrombocytopenia is generally more severe than leukopenia. However, both may be dose-limiting toxicities.
Lomustine may produce cumulative myelosuppression, manifested by more depressed indices or longer duration of suppression after repeated doses.
The occurrence of acute leukemia and bone marrow dysplasias have been reported in patients following long-term nitrosourea therapy.
Anemia also occurs, but is less frequent and less severe than thrombocytopenia or leukopenia.
Pulmonary Toxicity
Pulmonary toxicity characterized by pulmonary infiltrates and/or fibrosis has been reported rarely with Lomustine. Onset of toxicity has occurred after an interval of 6 months or longer from the start of therapy with cumulative doses of Lomustine usually greater than 1100 mg/m2. There is 1 report of pulmonary toxicity at a cumulative dose of only 600 mg.
Delayed onset pulmonary fibrosis occurring up to 17 years after treatment has been reported in patients who received related nitrosoureas in childhood and early adolescence (1–16 years) combined with cranial radiotherapy for intracranial tumors. There appeared to be some late reduction of pulmonary function of all long-term survivors. This form of lung fibrosis may be slowly progressive and has resulted in death in some cases. In this long-term study of carmustine, all those initially treated at less than 5 years of age died of delayed pulmonary fibrosis.
Gastrointestinal Toxicity
Nausea and vomiting may occur 3 to 6 hours after an oral dose and usually last less than 24 hours. Prior administration of antiemetics is effective in diminishing and sometimes preventing this side effect. Nausea and vomiting can also be reduced if Lomustine is administered to fasting patients.
Hepatotoxicity
A reversible type of hepatic toxicity, manifested by increased transaminase, alkaline phosphatase, and bilirubin levels, has been reported in a small percentage of patients receiving Lomustine.
Nephrotoxicity
Renal abnormalities consisting of progressive azotemia, decrease in kidney size, and renal failure have been reported in patients who received large cumulative doses after prolonged therapy with Lomustine. Kidney damage has also been reported occasionally in patients receiving lower total doses.
Other Toxicities
Stomatitis, alopecia, optic atrophy, and visual disturbances, such as blindness, have been reported infrequently.
Neurological reactions, such as disorientation, lethargy, ataxia, and dysarthria have been noted in some patients receiving Lomustine. However, the relationship to medication in these patients is unclear.
OVERDOSAGE
Accidental overdose with lomustine has been reported, including fatal cases. Accidental overdose has been associated with bone marrow suppression, abdominal pain, diarrhea, vomiting, anorexia, lethargy, dizziness, abnormal hepatic function, cough, and shortness of breath.
No proven antidotes have been established for Lomustine overdosage. In case of overdose, appropriate supportive measures should be taken.
DOSAGE AND ADMINISTRATION
The recommended dose of Lomustine in adult and pediatric patients as a single agent in previously untreated patients is 130 mg/m2 as a single oral dose every 6 weeks. In individuals with compromised bone marrow function, the dose should be reduced to 100 mg/m2 every 6 weeks. When Lomustine is used in combination with other myelosuppressive drugs, the doses should be adjusted accordingly. All doses of Lomustine must be rounded to the nearest 10 mg by the prescriber.
Doses subsequent to the initial dose should be adjusted according to the hematologic response of the patient to the preceding dose. The following schedule is suggested as a guide to dosage adjustment:
| Nadir After Prior Dose | Percentage of Prior Dose to be Given |
|
|---|---|---|
| Leukocytes (/mm3) | Platelets (/mm3) | |
| ≥4000 | ≥100,000 | 100% |
| 3000–3999 | 75,000–99,999 | 100% |
| 2000–2999 | 25,000–74,999 | 70% |
| <2000 | <25,000 | 50% |
A repeat course of Lomustine should not be given until circulating blood elements have returned to acceptable levels (platelets above 100,000/mm3; leukocytes above 4000/mm 3), and this is usually in 6 weeks. Adequate number of neutrophils should be present on a peripheral blood smear. Blood counts should be monitored weekly and repeat courses should not be given before 6 weeks because the hematologic toxicity is delayed and cumulative.
HOW SUPPLIED
Lomustine Capsules are available in individual bottles of 5 capsules each.
| 100 mg capsules (Green/Green) |
| 40 mg capsules (White/Green) |
| 10 mg capsules (White/White) |
Stability
Lomustine Capsules are stable for the lot life indicated on package labeling when stored in well-closed containers at 25°C (77°F); excursions permitted to 15°C–30°C (59°F–86°F) [see USP Controlled Room Temperature]. Avoid excessive heat (over 40°C, 104°F).
Directions to the Pharmacist
Confirm the total dose prescribed by the physician can be obtained by determining the appropriate combination of capsule strengths. Only the appropriate number of Lomustine capsules required for the administration of a single dose should be dispensed.
In order to provide the proper dose of Lomustine, patients should be aware that the prescribed dose may be made up of 2 or more different strengths and colors of capsules and that each strength must be dispensed separately. Inform patients that Lomustine is taken as a single oral dose and will not be repeated for at least 6 weeks. Daily use of the recommended dose may lead to toxicities and fatal outcomes.
Caution should be exercised when handling Lomustine Capsules. Procedures for proper handling and disposal of anticancer drugs should be utilized. Several guidelines on this subject have been published.1-4 To minimize the risk of dermal exposure, always wear impervious gloves when handling bottles containing Lomustine Capsules. Lomustine Capsules should not be broken. Personnel should avoid exposure to broken capsules. If contact occurs, wash immediately and thoroughly. More information is available in the references listed below.
REFERENCES
- NIOSH Alert: Preventing occupational exposures to antineoplastic and other hazardous drugs in healthcare settings. 2004. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 2004-165.
- OSHA Technical Manual, TED 1-0.15A, Section VI: Chapter 2. Controlling Occupational Exposure to Hazardous Drugs. OSHA, 1999. http://www.osha.gov/dts/osta/otm/otm_vi/otm_vi_2.html
- American Society of Health-System Pharmacists. ASHP guidelines on handling hazardous drugs. Am J Health-Syst Pharm. 2006;63:1172–1193.
- Polovich M, White JM, Kelleher LO, eds. 2005. Chemotherapy and biotherapy guidelines and recommendations for practice. 2nd ed. Pittsburgh, PA: Oncology Nursing Society.
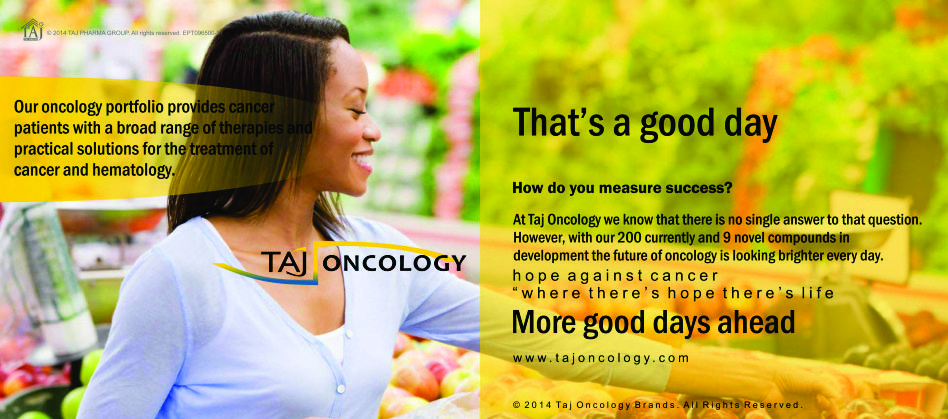
Product Glimpse
Description
We are committed to work towards a healthier and happier world. The company is an integrated, research based international pharmaceutical company, producing a wide range of quality, affordable generic (Lomustine 10mg/40mg/100mg Capsules) medicines, trusted by health-care professionals and patients across geographies.
We offer you the highest quality new Generic medicines ie. Lomustine 10mg/40mg/100mg Capsules, drugs and also with innovative packing at the lowest prices shipped to you from India. Browse our latest Pharmaceuticals and Generics possibilities and other pharmaceuticals possibilities…more.