Ifosfamide 1g Powder for Injection
Ifosfamide
1g Powder for Injection
Ifosfamide for injection is available in single-dose vials as follows:
1-gram Single-Dose Vial
3-gram Single-Dose Vial
Store at controlled room temperature 20°C to 25°C (68°F to 77°F).
Protect from temperatures above 30°C (86°F).
Exercise caution when handling Ifosfamide for Injection. The handling and preparation of ifosfamide should always be in accordance with current guidelines on safe handling of cytotoxic agents. Several guidelines on this subject have been published.1-4 Skin reactions associated with accidental exposure to Ifosfamide for Injection may occur. To minimize the risk of dermal exposure, always wear impervious gloves when handling vials and solutions containing Ifosfamide for Injection. If Ifosfamide for Injection solution contacts the skin or mucosa, immediately wash the skin thoroughly with soap and water or rinse the mucosa with copious amounts of water.
Ifosfamide for Injection is indicated for use in combination with certain other approved antineoplastic agents for third-line chemotherapy of germ cell testicular cancer. It should be used in combination with mesna for prophylaxis of hemorrhagic cystitis.
Ifosfamide
1g Powder for Injection
What Ifosfamide is and what it is used for
Ifosfamide is a cytotoxic drug or anti-cancer drug. It works by killing cancer cells, this is sometimes called ‘chemotherapy.
It is used to treat lots of different cancers. Ifosfamide is often used together with other anti-cancer drugs or radiotherapy.
Before you are given Ifosfamide
You will not be given Ifosfamide if:
- you have ever had an allergic reaction to Ifosfamide. An allergic reaction can include shortness of breath, wheezing, rash, itching or swelling of the face and lips
- your bone marrow is not working properly (especially if you have previously had chemotherapy or radiotherapy). You will have blood tests to check how well your bone marrow is working
- you have problems passing urine or a urinary tract infection, which can be recognised as pain when passing urine (cystitis)
- your liver and kidneys are not working properly. You will have blood tests to check this
- you currently have any infections
- you have ever had kidney or bladder problems as a result of previous chemotherapy or radiotherapy.
Tell your doctor if:
- you are already having, or have recently had, radiotherapy or chemotherapy
- you have diabetes
- you have kidney problems, including removal of a kidney
- you have been treated with cisplatin
- you have poor general health or are frail
- you are elderly.
If any of the above apply to you your doctor may need to do extra tests on your blood or urine and may decide to change your treatment.
Using other medicines and treatments
Tell your doctor or nurse if you are taking or have recently taken any other medicines, including medicines you have bought yourself.
In particular, tell them about the following medicines or treatments as they may not work well with Ifosfamide or may increase its side effects:
- medicines for diabetes taken by mouth called sulfonylureas, as they may lower your blood sugar more than usual when used with Ifosfamide
- medicines used to thin the blood such as warfarin. The risk of bleeding is increased when used with Ifosfamide
- a medicine used to treat gout called allopurinol
- an anti-cancer medicine called cisplatin
- an anti-viral medicine called acyclovir
- an anti-fungal medicine called amphotericin B
- certain sleeping tablets called barbiturates
- certain antibiotics such as streptomycin, gentamicin, amikacin and neomycin.
Effects on your blood and immune system
- Blood cells are made in your bone marrow. Three different types of blood cell are made:
- red blood cells, which carry oxygen around your body – white blood cells, which fight infection, and
- platelets, which help your blood to clot.
- After taking Ifosfamide, your blood count of the three types of cells will drop. This is an unavoidable side effect of Ifosfamide. Your blood count will reach its lowest level about 5 to 10 days after you start taking Ifosfamide and will stay low until a few days after you finish the course. Most people recover to a normal blood count within 21 to 28 days. If you have had a lot of chemotherapy in the past, it may take a little longer to return to normal.
- You may be more likely to get infections when your blood count drops. Try to avoid close contact with people who have coughs, colds and other infections.
- Your doctor will check that the number of red blood cells, white blood cells and platelets is high enough before and during your treatment with Ifosfamide.
Effects on your gums
It is important to keep your gums healthy, as mouth ulcers and infections can occur. Ask your doctor about this if you are unsure.
Effects on your bladder
- Ifosfamide can damage the lining of your bladder, causing bleeding into your urine. Your doctor knows this can happen and, if necessary, he or she will give you a medicine called Mesna which will protect your bladder.
- Mesna can either be given to you as a short injection, or mixed into the drip solution with your Ifosfamide, or as tablets.
- More information on Mesna can be found in the Patient Information Leaflet for Mesna Injection and Mesna tablets.
- Most people having Ifosfamide with Mesna do not develop any problems with their bladder, but your doctor may want to test your urine for the presence of blood using a ‘dipstick’ or microscope.
- If you notice that you have blood in the urine, you must tell your doctor straight away.
Effects on your kidneys
- Ifosfamide can damage your kidneys so that they do not work properly.
- This is more likely to happen if you only have one kidney or if your kidneys are already damaged.
- This is often temporary and they return to normal once Ifosfamide therapy is stopped. Occasionally the damage is permanent and more severe.
- Your doctor will check your test results for signs of kidney damage.
Contraception, pregnancy and breast-feeding
Do not become pregnant while taking Ifosfamide. This is because it can damage your unborn baby. Tell your doctor if you are pregnant, think you might be pregnant or are trying to become pregnant.
- Men or women should not try to have a child during treatment with or for at least 6 months after treatment. You should use an effective contraceptive. Ask your doctor for advice.
- Talk to your doctor about freezing sperm samples or eggs before your treatment starts.
Do not breast-feed while being treated with Ifosfamide. Ask your doctor for advice.
Driving or operating machines
Some of the side effects of treatment with Ifosfamide might affect your ability to drive and use machines safely. Your doctor will decide if it is safe for you to do so.
Turn over leaflet for further information.
What to do if you see a different doctor, or have to go to hospital
If you see any other doctor or have to go to hospital for any reason, tell them what medicines you are taking. Do not take any other medicines unless your doctor knows you are taking Ifosfamide.
How Ifosfamide is given
Ifosfamide will be given to you by a doctor or nurse.
- Ifosfamide will normally be added to a large bag of fluid and will be slowly injected (infused) directly in to your vein. The vein can be in your arm, the back of your hand or a large vein under your collar bone. Depending on your dose, the injection usually takes several hours but may be given over several days.
- Ifosfamide is often given with other anti-cancer drugs or radiotherapy.
The usual dose
- Your doctor will decide how much of the medicine you need and when you should take it.
- The amount of Ifosfamide you will need to take depends on: – the type of illness you have
- how big you are (a combination of your height and weight)
- your general health
- whether you are being given other anti-cancer drugs or having radiotherapy.
- Ifosfamide is usually given as a series of courses of treatment. After a course there is a break (a period when no tablets are taken) before the next course.
If you are given too much Ifosfamide
It is unlikely that you will be given more Ifosfamide than you should, because it will be given to you by a trained and qualified person. They would stop the injection straightaway if too much was given.
Possible side effects
Like all medicines, Ifosfamide can cause side effects, although not everybody gets them. The following side effects may happen with this medicine.
Tell your doctor straight away, if you notice any of the following serious side effects:
- getting bruises without knocking yourself, being slow to stop bleeding or bleeding from your nose or gums. This may be a sign that the platelet levels in your blood are getting too low a lowering of your white blood cell count, your doctor will check this during your treatment. It will not cause any signs, but you will be more likely to get infections. If you think you have an infection (a high temperature,
- feeling cold and shivery, or hot and sweaty, or any signs of infection such as a cough, or stinging on passing water) you may need antibiotics to fight infections because your blood count is lower than usual
- very pale, lethargic and tired. This may be a sign of low red blood cells (anaemia). Usually, no treatment is required, your body will eventually replace the red blood cells. If you are very anaemic, you may need a blood transfusion
- blood in your urine, pain, or less being passed.
- mental problems. In some people Ifosfamide can affect the brain. Sometimes people on Ifosfamide do not realise that they have been affected but friends and relatives may notice a change in them. If any of the following side effects are seen your doctor will stop your treatment with Ifosfamide.
- confusion
- drowsiness
- disorientation
- restlessness
- depression
- hallucinations
- muscle spasms in the arms or legs.
- rapid speech
- repeating words
- becoming clumsy
- fixed on a task
- aggression
- fits (convulsions)
- loss of consciousness.
These side effects may be accompanied by a fever or rapid heart beat.
Other possible side effects may be:
Digestive system
- feeling sick and being sick. This can last for about 24 hours after taking Ifosfamide. You may need to be given medicines to stop feeling or being sick. Ask your doctor about this
- diarrhoea
- constipation
- inflammation of the lining of your mouth including ulcers
- severe tummy and back pain (inflammation of the pancreas).
Skin and hair
- hair loss. You may just notice this as a little extra loss of hair when you are combing or washing your hair, or
- you may lose most or all of your hair. The amount of hair which you lose will depend on the dose of Ifosfamide, the thickness of your hair and whether you are also having
other anti-cancer drugs. If you are having Ifosfamide in combination with other anti-cancer drugs, you are
- much more likely to lose your hair than if you are having Ifosfamide alone
- yellowing of the skin or whites of eyes (jaundice), caused by liver problems
- skin rashes
- looking pale (anaemia), caused by a low red blood cell count. Your doctor will monitor this during your treatment
- bruising easily, caused by your blood clotting slowly
- changes in colour of your fingernails and skin
- worsening of skin problems due to radiotherapy.
Urinary
- burning sensation or pain when passing urine
- scarring and shrinkage of your bladder (pain and need to pass urine frequently)
- kidney problems, including failure.
Chest
- shortness of breath
- inflammation of your lungs which causes breathlessness, cough and raised temperature.
Heart and circulation
- inflammation in the vein at the site of treatment (thrombophlebitis)
- faster heart beat, heart failure
- changes in your heart rhythm and function with high doses, this would be seen on an electrocardiogram or ECG by your doctor.
Sexual
- no sperm count (in some cases, permanent)
- periods may be heavier than normal in women
- women’s periods stop (in some cases, permanently). Immune System
- allergic reactions, signs of this would be shortness of breath, wheezing, rash, itching or swelling of the face and lips.
General
- weakness
- loss of appetite
- secondary tumours (sometimes in the area of the bladder)
- bloating and swelling (water retention)
Changes can also be seen in the results of some tests on your blood:
- increased levels of certain chemicals called enzymes. If any of the side effects gets serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or nurse straight away.
How Ifosfamide is stored
Because Ifosfamide is usually given in hospital is will be stored safely and correctly by the hospital staff. If you do need the storage conditions they are given below.
- Keep out of the reach and sight of children.
- Do not use Ifosfamide after the expiry date which is stated on the label after EXP. The expiry date refers to the last day of that month.
- Do not store above 25ºC.
- Store in the original container.
Further information
What Ifosfamide contains
The active substance is Ifosfamide and each vial contains 1 g or 3 g.
There are no other ingredients.
What Ifosfamide looks like and contents of the pack
Ifosfamide is a dry white powder supplied in clear glass vials. Each carton contains 1 vial.
The contents of each vial has to be mixed with sterile water (called ‘water for injections’) before use.
1g combipack contains:
1 vial of ifosfamide
Ifosfamide
1g Powder for Injection
INDICATIONS AND USAGE
Ifosfamide for Injection is indicated for use in combination with certain other approved antineoplastic agents for third-line chemotherapy of germ cell testicular cancer. It should be used in combination with mesna for prophylaxis of hemorrhagic cystitis.
DOSAGE AND ADMINISTRATION
Ifosfamide for Injection should be administered intravenously at a dose of 1.2 grams per m2 per day for 5 consecutive days. Treatment is repeated every 3 weeks or after recovery from hematologic toxicity.
In order to prevent bladder toxicity, Ifosfamide for Injection should be given with extensive hydration consisting of at least 2 liters of oral or intravenous fluid per day. Mesna should be used to reduce the incidence of hemorrhagic cystitis. Ifosfamide for Injection should be administered as a slow intravenous infusion lasting a minimum of 30 minutes. Studies of Ifosfamide for Injection in patients with hepatic or renal impairment have not been conducted.
Injections are prepared for parenteral use by adding Sterile Water for Injection, USP or Bacteriostatic Water for Injection, USP (benzyl alcohol or parabens preserved), to the vial and shaking to dissolve. Before parenteral administration, the substance must be completely dissolved. Use the quantity of diluents shown below to constitute the product:
| Dosage Strength | Quantity of Diluent | Final Concentration |
|---|---|---|
| 1 gram | 20 mL | 50 mg per mL |
| 3 grams | 60 mL | 50 mg per mL |
Solutions of ifosfamide may be diluted further to achieve concentrations of 0.6 to 20 mg/mL in the following fluids:
- 5% Dextrose Injection, USP
- 0.9% Sodium Chloride Injection, USP
- Lactated Ringer's Injections, USP
- Sterile Water for Injection, USP
Because essentially identical stability results were obtained for Sterile Water admixtures as for the other admixtures (5% Dextrose Injection, 0.9% Sodium Chloride Injection, and Lactated Ringer’s Injection), the use of large volume parenteral glass bottles, Viaflex bags or PAB™ bags that contain intermediate concentrations or mixtures of excipients (e.g., 2.5% Dextrose Injection, 0.45% Sodium Chloride Injection, or 5% Dextrose and 0.9% Sodium Chloride Injection) is also acceptable.
Constituted or constituted and further diluted solutions of Ifosfamide for Injection should be refrigerated and used within 24 hours. Benzyl-alcohol-containing solutions can reduce the stability of ifosfamide.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
DOSAGE FORMS AND STRENGTHS
1 gram single-dose vial
3 gram single-dose vial
CONTRAINDICATIONS
Ifosfamide for Injection is contraindicated in patients with:
- Known hypersensitivity to administration of ifosfamide.
- Urinary outflow obstruction.
WARNINGS AND PRECAUTIONS
Myelosuppression, Immunosuppression, and Infections
Treatment with ifosfamide may cause myelosuppression and significant suppression of immune responses, which can lead to severe infections. Fatal outcomes of ifosfamide-associated myelosuppression have been reported. Ifosfamide-induced myelosuppression can cause leukopenia, neutropenia, thrombocytopenia (associated with a higher risk of bleeding events), and anemia. The nadir of the leukocyte count tends to be reached approximately during the second week after administration. When Ifosfamide for Injection is given in combination with other chemotherapeutic/hematotoxic agents and/or radiation therapy, severe myelosuppression is frequently observed. The risk of myelosuppression is dose-dependent and is increased with administration of a single high dose compared with fractionated administration. The risk of myelosuppression is also increased in patients with reduced renal function.
Severe immunosuppression has led to serious, sometimes fatal, infections. Sepsis and septic shock also have been reported. Infections reported with ifosfamide include pneumonias, as well as other bacterial, fungal, viral, and parasitic infections. Latent infections can be reactivated. In patients treated with ifosfamide, reactivation has been reported for various viral infections. Infections must be treated appropriately. Antimicrobial prophylaxis may be indicated in certain cases of neutropenia at the discretion of the managing physician. In case of neutropenic fever, antibiotics and/or antimycotics must be given. Close hematologic monitoring is recommended. White blood cell (WBC) count, platelet count and hemoglobin should be obtained prior to each administration and at appropriate intervals after administration. Unless clinically essential, Ifosfamide for Injection should not be given to patients with a WBC count below 2000/µL and/or a platelet count below 50,000/µL.
Ifosfamide for Injection should be given cautiously, if at all, to patients with presence of an infection, severe immunosuppression or compromised bone marrow reserve, as indicated by leukopenia, granulocytopenia, extensive bone marrow metastases, prior radiation therapy, or prior therapy with other cytotoxic agents.
Central Nervous System Toxicity, Neurotoxicity
Administration of ifosfamide can cause CNS toxicity and other neurotoxic effects. The risk of CNS toxicity and other neurotoxic effects necessitates careful monitoring of the patient. Neurologic manifestations consisting of somnolence, confusion, hallucinations, blurred vision, psychotic behavior, extrapyramidal symptoms, urinary incontinence, seizures, and in some instances, coma, have been reported following Ifosfamide for Injection therapy. There have also been reports of peripheral neuropathy associated with ifosfamide use.
Ifosfamide neurotoxicity may become manifest within a few hours to a few days after first administration and in most cases resolves within 48 to 72 hours of ifosfamide discontinuation. Symptoms may persist for longer periods of time. Supportive therapy should be maintained until their complete resolution. Occasionally, recovery has been incomplete. Fatal outcomes of CNS toxicity have been reported. Recurrence of CNS toxicity after several uneventful treatment courses has been reported. If encephalopathy develops, administration of ifosfamide should be discontinued.
Due to the potential for additive effects, drugs acting on the CNS (such as antiemetics, sedatives, narcotics, or antihistamines) must be used with particular caution or, if necessary, be discontinued in case of ifosfamide-induced encephalopathy.
Manifestations of CNS toxicity may impair a patient’s ability to operate an automobile or other heavy machinery.
Renal and Urothelial Toxicity and Effects
Ifosfamide is both nephrotoxic and urotoxic. Glomerular and tubular kidney function must be evaluated before commencement of therapy as well as during and after treatment. Monitor urinary sediment regularly for the presence of erythrocytes and other signs of uro/nephrotoxicity.
Monitor serum and urine chemistries, including phosphorus and potassium regularly. Administer appropriate replacement therapy as indicated. Renal parenchymal and tubular necrosis have been reported in patients treated with ifosfamide. Acute tubular necrosis, acute renal failure, and chronic renal failure secondary to ifosfamide therapy have been reported, and fatal outcome from nephrotoxicity has been documented.
Disorders of renal function, (glomerular and tubular) following ifosfamide administration are very common. Manifestations include a decrease in glomerular filtration rate, increased serum creatinine, proteinuria, enzymuria, cylindruria, aminoaciduria, phosphaturia, and glycosuria as well as tubular acidosis. Fanconi syndrome, renal rickets, and growth retardation in children as well as osteomalacia in adults also have been reported. Development of a syndrome resembling SIADH (syndrome of inappropriate antidiuretic hormone secretion) has been reported with ifosfamide.
Tubular damage may become apparent during therapy, months or even years after cessation of treatment. Glomerular or tubular dysfunction may resolve with time, remain stable, or progress over a period of months or years, even after completion of ifosfamide treatment.
The risk and expected benefits of ifosfamide therapy should be carefully weighed when considering the use of ifosfamide in patients with preexisting renal impairment or reduced nephron reserve.
Urotoxic side effects, especially hemorrhagic cystitis, have been very commonly associated with the use of Ifosfamide for Injection. These urotoxic effects can be reduced by prophylactic use of mesna.
Hemorrhagic cystitis requiring blood transfusion has been reported with ifosfamide. The risk of hemorrhagic cystitis is dose-dependent and increased with administration of single high doses compared to fractionated administration. Hemorrhagic cystitis after a single dose of ifosfamide has been reported. Past or concomitant radiation of the bladder or busulfan treatment may increase the risk for hemorrhagic cystitis.
Before starting treatment, it is necessary to exclude or correct any urinary tract obstructions.
During or immediately after administration, adequate amounts of fluid should be ingested or infused to force dieresis in order to reduce the risk of urinary tract toxicity. Obtain a urinalysis prior to each dose of Ifosfamide for Injection. If microscopic hematuria (greater than 10 RBCs per high power field) is present, then subsequent administration should be withheld until complete resolution. Further administration of Ifosfamide for Injection should be given with vigorous oral or parenteral hydration.
Ifosfamide should be used with caution, if at all, in patients with active urinary tract infections.
Cardiotoxicity
Manifestations of cardiotoxicity reported with ifosfamide treatment include:
- Supraventricular or ventricular arrhythmias, including atrial/supraventricular tachycardia, atrial fibrillation, pulseless ventricular tachycardia
- Decreased QRS voltage and ST-segment or T-wave changes
- Toxic cardiomyopathy leading to heart failure with congestion and hypotension
- Pericardial effusion, fibrinous pericarditis, and epicardial fibrosis
Fatal outcome of ifosfamide-associated cardiotoxicity has been reported.
The risk of developing cardiotoxic effects is dose-dependent. It is increased in patients with prior or concomitant treatment with other cardiotoxic agents or radiation of the cardiac region and, possibly, renal impairment.
Particular caution should be exercised when ifosfamide is used in patients with risk factors for cardiotoxicity and in patients with preexisting cardiac disease.
Pulmonary Toxicity
Interstitial pneumonitis, pulmonary fibrosis, and other forms of pulmonary toxicity have been reported with ifosfamide treatment. Pulmonary toxicity leading to respiratory failure as well as fatal outcome has also been reported. Monitor for signs and symptoms of pulmonary toxicity and treat as clinically indicated.
Secondary Malignancies
Treatment with ifosfamide involves the risk of secondary tumors and their precursors as late sequelae. The risk of myelodysplastic alterations, some progressing to acute leukemias, is increased. Other malignancies reported after use of ifosfamide or regimens with ifosfamide include lymphoma, thyroid cancer, and sarcomas.
The secondary malignancy may develop several years after chemotherapy has been discontinued.
Veno-occlusive Liver Disease
Veno-occlusive liver disease has been reported with chemotherapy that included ifosfamide.
Pregnancy
Ifosfamide for Injection can cause fetal harm when administered to a pregnant woman. Fetal growth retardation and neonatal anemia have been reported following exposure to ifosfamide-containing chemotherapy regimens during pregnancy. Ifosfamide is genotoxic and mutagenic in male and female germ cells. Embryotoxic and teratogenic effects have been observed in mice, rats and rabbits at doses 0.05 to 0.075 times the human dose.
Women should not become pregnant and men should not father a child during therapy with ifosfamide. Further, men should not father a child for up to 6 months after the end of therapy. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug or after treatment, the patient should be apprised of the potential hazard to a fetus.
Effects on Fertility
Ifosfamide interferes with oogenesis and spermatogenesis. Amenorrhea, azoospermia, and sterility in both sexes have been reported. Development of sterility appears to depend on the dose of ifosfamide, duration of therapy, and state of gonadal function at the time of treatment. Sterility may be irreversible in some patients.
Female Patients
Amenorrhea has been reported in patients treated with ifosfamide. The risk of permanent chemotherapy-induced amenorrhea increases with age. Pediatric patients treated with ifosfamide during prepubescence subsequently may not conceive and those who retain ovarian function after completing treatment are at increased risk of developing premature menopause.
Male Patients
Men treated with ifosfamide may develop oligospermia or azoospermia. Pediatric patients treated with ifosfamide during prepubescence might not develop secondary sexual characteristics normally, but may have oligospermia or azoospermia. Azoospermia may be reversible in some patients, though the reversibility may not occur for several years after cessation of therapy. Sexual function and libido are generally unimpaired in these patients. Some degree of testicular atrophy may occur. Patients treated with ifosfamide have subsequently fathered children.
Anaphylactic/Anaphylactoid Reactions and Cross-sensitivity
Anaphylactic/anaphylactoid reactions have been reported in association with ifosfamide. Cross-sensitivity between oxazaphosphorine cytotoxic agents has been reported.
Impairment of Wound Healing
Ifosfamide may interfere with normal wound healing.
Nursing
Ifosfamide is excreted in breast milk. Women must not breastfeed during treatment with ifosfamide [see Use in Specific Populations (8.3)].
ADVERSE REACTIONS
Adverse Reactions from Clinical Trials
Because clinical trials are conducted from widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice. The adverse reactions and frequencies below are based on 30 publications describing clinical experience with fractionated administration of ifosfamide as monotherapy with a total dose of 4 to 12 g/m2 per course.
|
||
| System Organ Class (SOC) | Adverse Reaction | Percentage (Ratio) |
|---|---|---|
| INFECTIONS AND INFESTATIONS | Infection |
9.9% (112/1128) |
| BLOOD AND LYMPHATIC SYSTEM DISORDERS | Leukopenia* (any) | --† |
|
Leukopenia <1 x 103/µL |
43.5% (267/614) |
|
| Thrombocytopenia‡ (any) | --§ | |
|
Thrombocytopenia ,50 x 103/µL |
4.8% (35/729) |
|
| Anemia¶ |
37.9% (202/533) |
|
| METABOLISM AND NUTRITION DISORDERS | Anorexia |
1.1% (15/1317) |
| NERVOUS SYSTEM DISORDERS | Central nervous system toxicity#,Þ |
15.4% (154/1001) |
| Peripheral neuropathy |
0.4% (5/1317) |
|
| CARDIAC DISORDERS | Cardiotoxicityß |
0.5% (7/1317) |
| VASCULAR DISORDERS | Hypotentionà |
0.3% (4/1317) |
| GASTROINTESTINAL DISORDERS | Nausea/Vomiting |
46.8% (443/964) |
| Diarrhea |
0.7% (9/1317) |
|
| Stomatitis |
0.3% (4/1317) |
|
| HEPATOBILIARY DISORDERS | Hepatotoxicityè |
1.8% (22/1190) |
| SKIN AND SUBCUTANEOUS TISSUES DISORDERS | Alopecia |
89.6% (540/603) |
| Dermatitis |
0.08% (1/1317) |
|
| Papular rash |
0.08% (1/1317) |
|
| RENAL AND URINARY DISORDERS | Hemorrhagic cystitis | --ð |
| Hematuria | ||
| - without mesna |
44.1% (282/640) |
|
| - with mesna |
21.3% (33/155) |
|
| Macrohematuria | ||
| - without mesna |
11.1% (66/594) |
|
| - with mesna |
5.2% (5/97) |
|
| Renal dysfunctionø | -- | |
| Renal structural damage | -- | |
| GENERAL DISORDERS AND ADMINISTRATIVE SITE CONDITIONS | Phlebitisý |
2.8% (37/1317) |
| Neutropenic fever£ |
1.0% (13/1317) |
|
| Fatigue |
0.3% (4/1317) |
|
| Malaise | Unable to calculate | |
Postmarketing Experience
The following adverse reactions have been reported in the post-marketing experience, listed by MedDRA System Organ Class (SOC), then by Preferred Term in order of severity, where feasible. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
INFECTIONS AND INFESTATIONS:
The following manifestations have been associated with myelosuppression and immunosuppression caused by ifosfamide: increased risk for and severity of infections†, pneumonias†, sepsis and septic shock (including fatal outcomes), as well as reactivation of latent infections, including viral hepatitis†, Pneumocystis jiroveci†, herpes zoster, Strongyloides, progressive multifocal leukoencephalopathy†, and other viral and fungal infections.
† Severe immunosuppression has led to serious, sometimes fatal, infections.
NEOPLASMS, BENIGN AND MALIGNANT AND UNSPECIFIED (INCL CYSTS AND POLYPS):
As treatment-related secondary malignancy*, Acute leukemia* (Acute myeloid leukemia)*, Acute promyelocytic leukemia*, Acute lymphocytic leukemia*, Myelodysplastic syndrome, Lymphoma (Non-Hodgkin’s lymphoma), Sarcomas*, Renal cell carcinoma, Thyroid cancer
BLOOD AND LYMPHATIC SYSTEM DISORDERS:
Hematotoxicity*, Myelosuppression manifested as Bone marrow failure, Agranulocytosis; Febrile bone marrow aplasia; Disseminated intravascular coagulation, Hemolytic uremic syndrome, Hemolytic anemia, Neonatal anemia, Methemoglobinemia
IMMUNE SYSTEM DISORDERS:
Angioedema*, Anaphylactic reaction, Immunosuppression, Urticaria, Hypersensitivity reaction
Syndrome of inappropriate antidiuretic hormone secretion (SIADH)
METABOLISM AND NUTRITION DISORDERS:
Tumor lysis syndrome, Metabolic acidosis, Hypokalemia, Hypocalcemia, Hypophosphatemia, Hyperglycemia, Polydipsia
PSYCHIATRIC DISORDERS:
Panic attack, Catatonia, Mania, Paranoia, Delusion, Delirium, Bradyphrenia, Mutism, Mental status change, Echolalia, Logorrhea, Perseveration, Amnesia
NERVOUS SYSTEM DISORDERS:
Convulsion*, Status epilepticus (convulsive and nonconvulsive), reversible posterior leukoencephalopathy syndrome, Leukoencephalopathy, Extrapyramidal disorder, Asterixis, Movement disorder, Polyneuropathy, Dysesthesia, Hypothesia, Paresthesia, Neuralgia, Gait disturbance, Fecal incontinence, Dysarthria
EYE DISORDERS:
Visual impairment, Vision blurred, Conjunctivitis, Eye irritation
EAR AND LABYRINTH DISORDERS:
Deafness, Hypoacusis, Vertigo, Tinnitus
CARDIAC DISORDERS:
Cardiotoxicity*, Cardiac arrest*, Ventricular fibrillation*, Ventricular tachycardia*, Cardiogenic shock*, Myocardial infarction*, Cardiac failure*, Bundle branch block left, Bundle branch block right, Pericardial effusion, Myocardial hemorrhage, Angina pectoris, Left ventricular failure, Cardiomyopathy*, Congestive cardiomyopathy, Myocarditis*, Arrhythmia*, Pericarditis, Atrial fibrillation, Atrial flutter, Bradycardia, Supraventricular extrasystoles, Premature atrial contractions, Ventricular extrasystoles, Myocardial depression, Palpitations, Ejection fraction decreased*, Electrocardiogram ST-segment abnormal, Electrocardiogram T-wave inversion, Electrocardiogram QRS complex abnormal
VASCULAR DISORDERS:
Pulmonary embolism, Deep vein thrombosis, Capillary leak syndrome, Vasculitis, Hypertension, Flushing, Blood pressure decreased
RESPIRATORY, THORACIC, AND MEDIASTINAL DISORDERS:
Respiratory failure*, Acute respiratory distress syndrome*, Pulmonary hypertension*, Interstitial lung disease* as manifested by Pulmonary fibrosis*, Alveolitis allergic, Interstitial pneumonitis, Pneumonitis*, Pulmonary edema*, Pleural effusion, Bronchospasm, Dyspnea, Hypoxia, Cough
GASTROINTESTINAL DISORDERS:
Cecitis, Colitis, Enterocolitis, Pancreatitis, Ileus, Gastrointestinal hemorrhage, Mucosal ulceration, Constipation, Abdominal pain, Salivary hypersecretion
HEPATOBILIARY DISORDERS:
Hepatic failure*, Hepatitis fulminant*, Veno-occlusive liver disease, Portal vein thrombosis, Cytolytic hepatitis, Cholestasis
SKIN AND SUBCUTANEOUS TISSUE DISORDERS:
Toxic epidermal necrolysis, Stevens-Johnson syndrome, Palmar-plantar erythrodysesthesia syndrome, Radiation recall dermatitis, Skin necrosis, Facial swelling, Petechiae, Macular rash, Rash, Pruritus, Erythema, Skin hyperpigmentation, Hyperhidrosis, nail disorder
MUSCULOSKELETAL AND CONNECTIVE TISSUE DISORDER:
Rhabdomyolysis, Osteomalacia, Rickets, Growth retardation, Myalgia, Arthralgia, Pain in extremity, Muscle twitching
RENAL AND URINARY DISORDERS:
Fanconi syndrome, Tubulointerstitial nephritis, Nephrogenic diabetes insipidus, Phosphaturia, Aminoaciduria, Polyuria, Enuresis, Feeling of residual urine
Fatal outcomes from acute and chronic renal failure have been documented.
REPRODUCTIVE SYSTEM AND BREAST DISORDERS:
Infertility, Ovarian failure, Premature menopause, Amenorrhea, Ovarian disorder, Ovulation disorder, Azoospermia, Oligospermia, Impairment of spermatogenesis, Blood estrogen decreased, Blood gonadotrophin increased
CONGENITAL, FAMILIAL AND GENETIC DISORDERS:
Fetal growth retardation
GENERAL DISORDERS AND ADMINISTRATIVE SITE CONDITIONS:
Multi-organ failure*, General physical deterioration, Injection/Infusion site reactions including swelling, inflammation, pain, erythema, tenderness, pruritus; Chest pain, Edema, Mucosal inflammation, Pain, Pyrexia, Chills
* Including fatal outcomes
DRUG INTERACTIONS
Ifosfamide is a substrate for both CYP3A4 and CYP2B6.
Inducers of CYP3A4
CYP3A4 inducers (e.g., carbamazepine, phenytoin, fosphenytoin, phenobarbital, rifampin, St. John Wort) may increase the metabolism of ifosfamide to its active alkylating metabolites. CYP3A4 inducers may increase the formation of the neurotoxic/nephrotoxic ifosfamide metabolite, chloroacetaldehyde. Closely monitor patients taking ifosfamide with CYP3A4 inducers for toxicities and consider dose adjustment.
Inhibitors of CYP3A4
CYP3A4 inhibitors (e.g., ketoconazole, fluconazole, itraconazole, sorafenib, aprepitant, fosaprepitant, grapefruit, grapefruit juice) may decrease the metabolism of ifosfamide to its active alkylating metabolites, perhaps decreasing the effectiveness of ifosfamide treatment. CYP 3A4 inhibitors may also decrease the formation of an ifosfamide neurotoxic/nephrotoxic metabolite, chloroacetaldehyde.
USE IN SPECIFIC POPULATIONS
Pregnancy
Pregnancy Category D
[See Warnings and Precautions].
Ifosfamide for Injection can cause fetal harm when administered to a pregnant woman. Fetal growth retardation and neonatal anemia have been reported following exposure to ifosfamide-containing chemotherapy regimens during pregnancy.
Animal studies indicate that ifosfamide is capable of causing gene mutations and chromosomal damage in vivo. In pregnant mice, resorptions increased and anomalies were present at day 19 after a 30 mg/m2 dose of ifosfamide was administered on day 11 of gestation. Embryo-lethal effects were observed in rats following the administration of 54 mg/m2 doses of ifosfamide from the 6th through the 15th day of gestation and embryotoxic effects were apparent after dams received 18 mg/m2 doses over the same dosing period. Ifosfamide is embryotoxic to rabbits receiving 88 mg/m2/day doses from the 6th through the 18th day after mating. The number of anomalies was also significantly increased over the control group.
Women should not become pregnant and men should not father a child during therapy with ifosfamide. Further, men should not father a child for up to 6 months after the end of therapy. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug or after treatment, the patient should be apprised of the potential hazard to a fetus.
Nursing Mothers
Ifosfamide is excreted in breast milk. Because of the potential for serious adverse events and the tumorigenicity shown for ifosfamide in animal studies, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. Women must not breastfeed during treatment with ifosfamide.
Pediatric Use
Safety and effectiveness have not been established in pediatric patients.
Geriatric Use
In general, dose selection for an elderly patient should be cautious, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
A study of patients 40 to 71 years of age indicated that elimination half-life appears to increase with advancing age. This apparent increase in half-life appeared to be related to increases in volume of distribution of ifosfamide with age. No significant changes in total plasma clearance or renal or non-renal clearance with age were reported.
Ifosfamide and its metabolites are known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
Use in Patients with Renal Impairment
No formal studies were conducted in patients with renal impairment. Ifosfamide and its metabolites are known to be excreted by the kidneys and may accumulate in plasma with decreased renal function. Patients with renal impairment should be closely monitored for toxicity and dose reduction may be considered. Ifosfamide and its metabolites are dialyzable.
Use in Patients with Hepatic Impairment
No formal studies were conducted in patients with hepatic impairment. Ifosfamide is extensively metabolized in the liver and forms both efficacious and toxic metabolites. Ifosfamide for Injection should be given cautiously to patients with impaired hepatic function.
OVERDOSAGE
No specific antidote for Ifosfamide for Injection is known.
Patients who receive an overdose should be closely monitored for the development of toxicities. Serious consequences of overdosage include manifestations of dose-dependent toxicities such as CNS toxicity, nephrotoxicity, myelosuppression, and mucositis.
Management of overdosage would include general supportive measures to sustain the patient through any period of toxicity that might occur, including appropriate state-of-the-art treatment for any concurrent infection, myelosuppression, or other toxicity. Ifosfamide as well as ifosfamide metabolites are dialyzable.
Cystitis prophylaxis with mesna may be helpful in preventing or limiting urotoxic effects with overdose.
DESCRIPTION
Ifosfamide for Injection (ifosfamide for injection, USP) single-dose vials for constitution and administration by intravenous infusion each contain 1 gram or 3 grams of sterile ifosfamide. Ifosfamide is a chemotherapeutic agent chemically related to the nitrogen mustards and a synthetic analog of cyclophosphamide. Ifosfamide is 3-(2-chloroethyl)-2-[(2-chloroethyl)amino]tetrahydro-2H-1,3,2-oxazaphosphorine 2-oxide. The molecular formula is C7H15Cl2N2O2P and its molecular weight is 261.1. Ifosfamide is a white crystalline powder soluble in water. There are no excipients in the formulation. Each vial contains 1 gram or 3 grams of sterile ifosfamide alone.
Its structural formula is:

CLINICAL PHARMACOLOGY
Mechanism of Action
Ifosfamide is a prodrug that requires metabolic activation by hepatic cytochrome P450 isoenzymes to exert its cytotoxic activity. Activation occurs by hydroxylation at the ring carbon atom forming the unstable intermediate 4-hydroxyifosfamide and its ring-opened aldo tautomer, which decomposes to yield the cytotoxic and urotoxic compound acrolein and an alkylating isophosphoramide mustard as well as multiple other nontoxic products. The exact mechanism of action of ifosfamide has not been determined, but its cytotoxic action is primarily through DNA crosslinks caused by alkylation by the isophosphoramide mustard at guanine N-7 positions. The formation of inter- and intra-strand cross-links in the DNA results in cell death.
Pharmacokinetics
Ifosfamide exhibits dose-dependent pharmacokinetics in humans. At single doses of 3.8 to 5.0 g/m2, the plasma concentrations decay biphasically and the mean terminal elimination half-life is about 15 hours. At doses of 1.6 to 2.4 g/m2/day, the plasma decay is monoexponential and the terminal elimination half-life is about 7 hours.
Ifosfamide exhibits time-dependent pharmacokinetics in humans. Following intravenous administration of 1.5 g/m2 over 0.5 hour once daily for 5 days to 15 patients with neoplastic disease, a decrease in the median elimination half-life from 7.2 hour on Day 1 to 4.6 hours on Day 5 occurred with a concomitant increase in the median clearance from 66 mL/min on Day 1 to 115 mL/min on Day 5. There was no significant change in the volume of distribution on Day 5 compared with Day 1.
Distribution
Ifosfamide volume of distribution (Vd) approximates the total body water volume, suggesting that distribution takes place with minimal tissue binding. Following intravenous administration of 1.5 g/m2 over 0.5 hour once daily for 5 days to 15 patients with neoplastic disease, the median Vd of ifosfamide was 0.64 L/kg on Day 1 and 0.72 L/kg on Day 5. Ifosfamide shows little plasma protein binding. Ifosfamide and its active metabolites are extensively bound by red blood cells. Ifosfamide is not a substrate for P-glycoprotein.
Metabolism
Ifosfamide is extensively metabolized in humans through two metabolic pathways: ring oxidation ("activation") to form the active metabolite, 4-hydroxy-ifosfamide and side-chain oxidation to form the inactive metabolites, 3-dechloro-ethylifosfamide or 2-dechloroethylifosfamide with liberation of the toxic metabolite, chloroacetaldehyde. Small quantities (nmol/mL) of ifosfamide mustard and 4-hydroxyifosfamide are detectable in human plasma. Metabolism of ifosfamide is required for the generation of the biologically active species and while metabolism is extensive, it is also quite variable among patients.
Excretion
After administration of doses of 5 g/m2 of 14C-labeled ifosfamide, from 70% to 86% of the dosed radioactivity was recovered in urine as metabolites, with about 61% of the dose excreted as parent compound. At doses of 1.6 to 2.4 g/m2 only 12% to 18% of the dose was excreted in the urine as unchanged drug within 72 hours. Two different dechloroethylated derivatives of ifosfamide, 4-carboxyifosfamide, thiodiacetic acid and cysteine conjugates of chloroacetic acid have been identified as the major urinary metabolites of ifosfamide in humans and only small amounts of 4-hydroxyifosfamide and acrolein are present.
Pediatrics
Population PK analysis was performed on plasma data from 32 pediatric patients various malignant diseases aged between 1 and 18 years. Patients received a total of 45 courses of ifosfamide at doses of 1.2, 2.0 and 3.0 g/m2 given intravenously over 1 or 3 hours on 1, 2, or 3 days. The mean±standard error population estimates for the initial clearance and volume of distribution of ifosfamide were 2.4±0.33 L/h/m2 and 21±1.6 L/m2 with an interindividual variability of 43% and 32%, respectively.
Effect of Age
A study of 20 patients between 40 to 71 years of age receiving 1.5 g/m2 of ifosfamide daily for 3 or 5 days indicated that elimination half-life appears to increase with age. The elimination half-life increase appeared to be related to the increase in ifosfamide volume of distribution with age. No significant changes in total plasma clearance or renal clearance with age were reported.
NONCLINICAL TOXICOLOGY
Carcinogenesis, Mutagenesis, Impairment of Fertility
Ifosfamide has been shown to be carcinogenic in rats when administered by intraperitoneal injection at 6 mg/kg (37 mg/m2, or about 3% of the daily human dose on a mg/m2 basis) 3 times a week for 52 weeks. Female rats had a significantly higher incidence of uterine leiomyosarcomas and mammary fibroadenomas than vehicle controls.
The mutagenic potential of ifosfamide has been documented in bacterial systems in vitro and mammalian cells in vivo. In vivo, ifosfamide has induced mutagenic effects in mice and Drosophila melanogaster germ cells, and has induced a significant increase in dominant lethal mutations in male mice as well as recessive sex-linked lethal mutations in Drosophila.
Ifosfamide was administered to male and female beagle dogs at doses of 1.00 or 4.64 mg/kg/day (20 or 93 mg/m2) orally 6 days a week for 26 weeks. Male dogs at 4.64 mg/kg (about 7.7% of the daily clinical dose on a mg/m2 basis) had testicular atrophy with degeneration of the seminiferous tubular epithelium. In a second study, male and female rats were given 0, 25, 50, or 100 mg/kg (0, 150, 300, or 600 mg/m2) ifosfamide intraperitoneally once every 3 weeks for 6 months. Decreased spermatogenesis was observed in most male rats given 100 mg/kg (about half the daily clinical dose on a mg/m2 basis).
CLINICAL STUDIES
Patients with refractory testicular cancer (n=59) received a combination of ifosfamide, cisplatin, and either etoposide (VePesid®) or vinblastine (VIP) as third-line therapy or later. The selection of etoposide or vinblastine (“V” in the VIP regimen) was guided by the therapeutic effect achieved with prior regimens. The contribution of ifosfamide to the VIP combination was determined in patients treated with cisplatin-etoposide prior to ifosfamide- cisplatin-etoposide or those who received cisplatin-vinblastine prior to ifosfamide-cisplatin-vinblastine.
A total of 59 patients received a third-line salvage regimen which consisted of ifosfamide 1.2 g/m2/day intravenously on days 1 to 5, cisplatin 20 mg/m2/day intravenously on days 1 to 5, and either etoposide 75 mg/m2/day intravenously on days 1 to 5 or vinblastine 0.22 mg/kg intravenously on day 1. Efficacy results with the VIP regimen were compared to data pooled from six single agent phase II trials conducted between August 1980 and October 1985 including a total of 90 patients of whom 65 were eligible as controls of this study. Twenty-three patients in the VIP regimen became free of disease with VIP alone or VIP plus surgery, whereas a single patient in the historical control group achieved complete response. The median survival time exceeded two years in the VIP group versus less than one year in the control group. Performance status ≥ 80, embryonal carcinoma and minimal disease were favorable prognostic factors for survival. In all prognostic categories, the difference between VIP and historical controls remained highly significant.
|
|||
| Number. (%) of Patients | |||
|---|---|---|---|
| VIP | Control | p-value | |
| Total Patients | 59 (100) | 65 (100) | |
| Disease-free | 23 (39) | 1 (2) | < 0.001 |
| Chemotherapy alone | 15 (25) | 1 (2) | < 0.001 |
| Chemotherapy plus surgery | 8 (14) | 0 | |
| Overall Response | 32 (54) | 2 (3) | < 0.001 |
| Time to progression (weeks) | |||
| Median | 19 | 4 | < 0.001* |
| Range | 1 – 205+ | 1 – 29 | |
| Disease-free interval (weeks) | |||
| Median | 114 | 29 | |
| Range | 13 – 205+ | -- | |
| Survival (weeks) | |||
| Median | 53 | 10 | < 0.001* |
| Range | 1 – 205+ | 1 – 123+ | |
In a study, 50 fully evaluable patients with germ cell testicular cancer were treated with Ifosfamide for Injection in combination with cisplatin and either vinblastine or etoposide after failing (47 of 50 patients) at least two prior chemotherapy regimens consisting of cisplatin/vinblastine/bleomycin, (PVB), cisplatin/vinblastine/actinomycin D/bleomycin/cyclophosphamide, (VAB6), or the combination of cisplatin and etoposide. Patients were selected for remaining cisplatin sensitivity because they had previously responded to a cisplatin containing regimen and had not progressed while on the cisplatin containing regimen or within 3 weeks of stopping it. Patients served as their own control based on the premise that long term complete responses could not be achieved by retreatment with a regimen to which they had previously responded and subsequently relapsed.
Ten of 50 fully evaluable patients were still alive 2 to 5 years after treatment. Four of the 10 long term survivors were rendered free of cancer by surgical resection after treatment with the ifosfamide regimen; median survival for the entire group of 50 fully evaluable patients was 53 weeks.
15 REFERENCES
- NIOSH Alert: Preventing occupational exposures to antineoplastic and other hazardous drugs in healthcare settings. 2004. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 2004-165.
- OSHA Technical Manual, TED 1-0.15A, Section VI: Chapter 2. Controlling occupational exposure to hazardous drugs. OSHA, 1999. http://www.osha.gov/dts/osta/otm/otm_vi/otm_vi_2.html
- American Society of Health-System Pharmacists. ASHP guidelines on handling hazardous drugs. Am J Health-Syst Pharm. 2006; 63:1172-1193.
- Polovich M, White JM, Kelleher LO, (eds.) 2005. Chemotherapy and biotherapy guidelines and recommendations for practice. (2nd ed.) Pittsburgh, PA: Oncology Nursing Society.
HOW SUPPLIED/STORAGE AND HANDLING
Ifosfamide for injection is available in single-dose vials as follows:
1-gram Single-Dose Vial
3-gram Single-Dose Vial
Store at controlled room temperature 20°C to 25°C (68°F to 77°F).
Protect from temperatures above 30°C (86°F).
Exercise caution when handling Ifosfamide for Injection. The handling and preparation of ifosfamide should always be in accordance with current guidelines on safe handling of cytotoxic agents. Several guidelines on this subject have been published.1-4 Skin reactions associated with accidental exposure to Ifosfamide for Injection may occur. To minimize the risk of dermal exposure, always wear impervious gloves when handling vials and solutions containing Ifosfamide for Injection. If Ifosfamide for Injection solution contacts the skin or mucosa, immediately wash the skin thoroughly with soap and water or rinse the mucosa with copious amounts of water.
PATIENT COUNSELING INFORMATION
Inform patients of the risks associated with the use of Ifosfamide for Injection as well as the plan for regular blood monitoring during therapy.
Specifically inform patients of the following:
- Treatment with ifosfamide may cause myelosuppression which can be severe and lead to fatal outcome. Significant suppression of immune responses can also occur which can lead to severe infections. Latent infections can be reactivated. Patients should report fever or other symptoms of an infection.
- The risk of bleeding and anemia.
- The risk of CNS toxicity and other neurotoxic effects with fatal outcome.
- The risk of bladder and kidney toxicity. Patients should be aware of the need to increase fluid intake and frequent voiding to prevent accumulation in the bladder.
- The risk of cardiotoxicity and fatal outcome. Patients should report preexisting cardiac disease.
- The risk of pulmonary toxicity leading to respiratory failure with fatal outcome.
- The risk of secondary malignancies due to therapy.
- The risk of veno-occlusive liver disease.
- The potential hazard to a fetus if a patient becomes pregnant or fathers a child during therapy and for up to 6 months after therapy. Effective methods of contraception should be used during therapy and for up to 6 months after therapy.
- The potential for serious adverse reactions and tumorigenicity when children are breastfed during therapy.
- The risk of amenorrhea, premature menopause, and sterility.
- The risk of alopecia, wound healing, and other serious skin and subcutaneous tissue disorders.
- Therapy may cause gastrointestinal disorders and alcohol may increase nausea and vomiting.
- The risk of stomatitis and the importance of proper oral hygiene.
- The risk of eye disorders such as visual impairment, blurred vision, and eye irritation.
- The risk of ear and labyrinth disorders such as deafness, vertigo, and tinnitus.
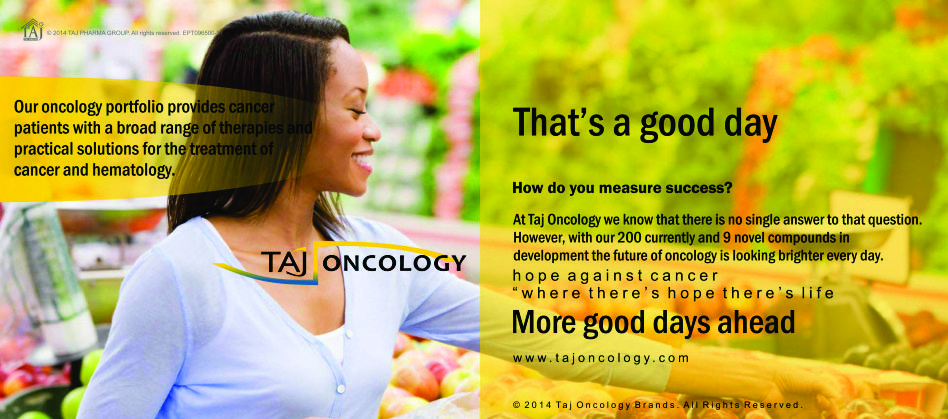
Product Glimpse
Description
We are committed to work towards a healthier and happier world. The company is an integrated, research based international pharmaceutical company, producing a wide range of quality, affordable generic (Ifosfamide 1g Powder for Injection) medicines, trusted by health-care professionals and patients across geographies.
We offer you the highest quality new Generic medicines ie. Ifosfamide 1g Powder for Injection, drugs and also with innovative packing at the lowest prices shipped to you from India. Browse our latest Pharmaceuticals and Generics possibilities and other pharmaceuticals possibilities…more.