Ibritumomab tiuxetan 3.2mg/2ml Injection
Ibritumomab Tiuxetan
3.2mg/2ml Injection
A kit is used for preparing Y-90 radiolabeled Ibritumomab Tiuxetan (NDC 68152-103-03). The contents of all vials are sterile, pyrogen-free, contain no preservatives, and are not radioactive. The kit contains four identification labels and the following four vials:
One (1) Ibritumomab Tiuxetan vial containing 3.2 mg ibritumomab tiuxetan in 2 mL 0.9% Sodium Chloride as a clear, colorless solution.
One (1) 50 mM Sodium Acetate Vial containing 13.6 mg Sodium Acetate trihydrate in 2 mL Water for Injection, USP as a clear, colorless solution.
One (1) Formulation Buffer Vial containing 750 mg Albumin (Human), 76 mg Sodium Chloride, 28 mg Sodium Phosphate Dibasic Dodecahydrate, 4 mg Pentetic Acid, 2 mg Potassium Phosphate Monobasic and 2 mg Potassium Chloride in 10 mL Water for Injection, pH 7.1 as a clear yellow to amber colored solution.
One (1) empty Reaction Vial.
Yttrium-90 Chloride Sterile Solution is shipped directly from the supplier upon placement of an order for the Y-90 Ibritumomab Tiuxetan kit.
- Keep out of the reach and sight of children.
- Do not use Ibritumomab after the expiry date which is stated on the pack.
- This medicine will be stored by a healthcare professional.
Store in a refrigerator (2°C - 8°C). Do not freeze. Store the vials in the original package in order to protect from light. Storage must be in accordance with national regulations for radioactive materials. - After radiolabelling, an immediate use is recommended. Stability has been demonstrated for 8 hours at 2°C - 8°C and protected from light.
Ibritumomab Tiuxetan
3.2mg/2ml Injection
What is it and how is it used?
- The preparation of the active substance Ibritumomab tiuxetan [ Y], a monoclonal antibody labelled with the radioactive substance yttrium-90 ( Y). Ibritumomab attaches to a protein (CD20) on the surface of certain white blood cells (B-cells) and kills them by irradiation.
- Ibritumomab is used to treat patients suffering from specific subgroups of B-cell non-Hodgkin’s lymphoma (CD20+ indolent or transformed B-cell NHL) if an earlier rituximab, another monoclonal antibody, treatment has not worked, or has stopped working (refractory or relapsed disease).
- Ibritumomab is also used in previously untreated patients with follicular lymphoma. It is used as a consolidation therapy to improve the reduction in the number of lymphoma cells (remission) achieved with the initial chemotherapy regimen.
What do you have to consider before using it?
You must not be given Ibritumomab :
- if you are allergic (hypersensitive) to any of the following: - ibritumomab tiuxetan, yttrium chloride or to any of the other ingredients of Ibritumomab (listed in section 6 ‘What Ibritumomab contains’) - rituximab or other murine-derived proteins
- if you are pregnant or breast-feeding (see also section “pregnancy and breast feeding”).
Take special care with Ibritumomab Tiuxetan
In the following cases, Ibritumomab Tiuxetan use is not recommended since its safety and efficacy have not been established
- more than a quarter of your bone marrow contains malignant abnormal cells.
- If you have had external beam radiation a type of radiotherapy to more than a quarter of your bone marrow.
- If you receive Ibritumomab Tiuxetan alone and the number of your blood platelets is fewer than 100,000mm3
- If the number of your blood platelets is fewer than 150,000mm3 after chemotherapy
- If the number of your white blood cells is fewer than 1,500mm3
- If you have had a bone marrow transplant or have received blood stem cells in the past.
If you have been treated with other proteins (especially mouse-derived) before Ibritumomab treatment, you may be more likely to have an allergic reaction. You may, therefore, need to be tested for special antibodies.
In addition, Ibritumomab is not recommended for the use in patients with non-Hodgkin’s lymphoma involving the brain and/or spinal cord as those patients were not included in clinical studies.
Children:
Ibritumomab is not recommended for use in children below age 18 since safety and efficacy have not been established.
Elderly patients:
Limited data in elderly patients (aged 65 years or over) are available. No overall differences in safety or efficacy were observed between these patients and younger patients.
Using other medicines
Please tell your doctor or pharmacist if you are using or have recently used any other medicines, including medicines obtained without a prescription.
In particular, your doctor will need to interrupt treatment with growth factors such as filgrastim for a period of three weeks before giving you Ibritumomab to two weeks after Ibritumomab treatment. If you are given Ibritumomab less than 4 months after chemotherapy containing the active substance fludarabine, you may have a higher risk of having a reduced number of blood cells. Please tell your doctor that you were given Ibritumomab if you are due for vaccination after using it.
Pregnancy and breast-feeding
Ibritumomab must not be used during pregnancy. Your doctor will perform tests to exclude pregnancy before you start the treatment. Women of child-bearing potential and male patients must use reliable contraception during treatment with Ibritumomab and for up to one year after stopping treatment. There is a potential risk that ionizing radiation by Ibritumomab could harm your ovaries and testicles. Please ask your doctor how this may affect you, especially if you are planning on having children in the future.
Women must not breast-feed during treatment and for 12 months following the treatment. .
Driving and using machines
Ibritumomab can affect your abilityto drive and use machines, as dizziness is a common side effect. Please be cautious until you are sure you are not affected.
Important information about some of the ingredients of Ibritumomab
This medicine contains up to 28 mg sodium per dose, depending on the radioactivity concentration. To be taken into consideration by patients on a controlled sodium diet.
How is it used?
Ibritumomab must be handled and administered by experienced professionals in a medical facility authorized to use radioactive medicines.
The dose of Ibritumomab depends on your body weight, blood platelet counts and what Ibritumomab is being used for (indication). The maximum dose must not exceed 1200 MBq (‘megabecquerel’, a unit to measure radioactivity).
Ibritumomab is used with another medicine containing the active substance rituximab.
You will be given a total of 3 infusions in the course of two visits to a medical facility, 7 to 9 days apart.
- On day 1 you will be given one rituximab infusion
- On day 7, 8, or 9 you will be given one rituximab infusion, followed by one Ibritumomab infusion shortly afterwards (within 4 hours).
How much Ibritumomab is given
For consolidation therapy in patients with follicular lymphoma
The usual dose is 15 MBq/kg body weight.
For therapy of patients with relapsed or refractory Non-Hodgkin’s lymphoma not responding to rituximab
The usual dose is 11 or 15 MBq per kg body weight, depending on your blood platelet count.
Preparation of Ibritumomab
Ibritumomab is not used directly, but must be prepared by your healthcare professional first. The kit allows the coupling of antibody ibritumomab tiuxetan with the radioactive isotope yttrium Y (radiolabelling).
How Ibritumomab is given
Ibritumomab is given by intravenous infusion (drip into a vein) usually lasting about 10 minutes.
After you are given Ibritumomab
The amount of radiation that your body will be exposed to due to Ibritumomab is smaller than with radiotherapy. Most radioactivity will decay within the body, but a small part will be eliminated through your urine. Therefore, for one week after the Ibritumomab infusion you must wash your hands thoroughly each time after urinating.
After treatment your doctor will perform regular blood tests to check your platelet and white cell counts. These usually decrease around two months after start of treatment.
If your doctor plans to treat you with some other antibody after treatment with Ibritumomab , you will need to be tested for special antibodies. Your doctor will tell you if this applies to you.
If you have received more Ibritumomab than you should
Your doctor will treat you, as appropriate, if you have any particular ill effects. This may include discontinuation of Ibritumomab therapy and treatment with growth factors or your own stem cells.
What are possible side effects?
Like all medicines, Ibritumomab can cause side effects, although not everybody gets them.
Tell your doctor immediately if you notice symptoms of any of the following:
- infection: fever, chills
- blood poisoning (sepsis): fever and chills, changes in mental status, rapid breathing, increased heart rate, decreased urine output, low blood pressure, shock, problems with bleeding or clotting
- infections of the lung (pneumonia): breathing difficulties
- Low counts of blood cells: unusual bruising, more bleeding then usual after injury, fever, or if you feel unusually tired or breathless
- severe mucous membrane reactions, which may occur days or months after Ibritumomab Tiuxetan andor rituximab administration. Your doctor will immediately stop the treatment.
- extravasation (leakage of the infusion to the surrounding tissue): pain, burning sensation, stinging or another reaction at the infusion site during administration. Your doctor will immediately stop the infusion and restart it using another vein.
- allergic (hypersensitivity) reactionsinfusion reactions: symptoms for allergic reactions infusion reactions may be skin reactions, breathing difficulties, swelling, itching, flushing, chills, dizziness as potential sign for low blood pressure. Depending on the kindseverity of reaction your doctor will decide if treatment must be stopped immediately.
Side effects may occur with certain frequencies, which are defined as follows:
- very common: occur in at least 1 in 10 patients
- common: occur in at least 1 in 100 patients but less than 1 in 10 patients
- uncommon: occur in at least 1 in 1,000 patients but less than 1 in 100
- patients - rare: occur in at least 1 in 10,000 patients but less than 1 in 1,000 patients
- very rare: occur in less than 1 in 10,000 patients
- not known: frequency cannot be estimated from the available data.
The side effects marked with an asterisk (*) have led to death in some cases, either in clinical trials or during the marketing of the product.
The side effects marked with two asterisks (**) were observed additionally under consolidation therapy.
Very common side effects
- decreased number of blood platelets, white and red blood cells ( thrombocytopenia, leukocytopenia, neutropenia, anaemia )*
- feeling sick (nausea)
- weakness, fever, chills (rigor)
- infection*
- tiredness**
- red pinpoint spots under the skin ( petechia)**
Common side effects
- blood poisoning ( sepsis)*; infection of the lungs (pneumonia)*; urinary tract infection, fungal infections in the mouth such as oral thrush ( oral candidiasis)
- other blood related cancers ( myelodysplastic syndrome (MDS) / acute myeloid leukaemia (AML)) *; tumour pain
- fever with decrease in the number of specific white blood cells (febrile neutropenia); decreased counts of all blood cells (pancytopenia)*; decreased number of lymphocytes (lymphocytopenia)
- allergic ( hypersensitivity) reactions
- severe loss of appetite (anorexia)
- feeling anxious ( anxiety); trouble sleeping ( insomnia)
- dizziness; headache,
- bleeding due to decreased blood platelet counts*,
- cough; runny nose
- vomiting, stomach ( abdominal) pain; diarrhoea; indigestion; throat irritation; constipation
- rash; itching ( pruritus)
- joint pain ( arthralgia) aching muscles ( myalgia); back pain; neck pain
- pain; flu-like symptoms; generally feeling unwell ( malaise), swelling caused by build-up of fluid in the arms and legs and other tissues ( peripheral oedema); increased sweating
- high blood pressure ( hypertension)**
- low blood pressure ( hypotension)**
- absence of menstruation (amenorrhea)**
Uncommon side effects:
- rapid heart beat ( tachycardia),
Rare side effects:
- benign brain tumour ( meningioma),
- bleeding in the head due to decreased blood platelet counts*,
Side effects for which frequency is not known:
- reaction of the skin and mucous membranes (including Stevens-Johnson Syndrome) *
- leakage of the infusion to the surrounding tissue ( extravasation), causing skin inflammation (infusion site dermatitis) and shedding ( infusion site desquamation) or injection site ulcers
- tissue damage around tumours of the lymph system and complications due to swelling of such tumours
If any of the side effects gets serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist.
What happens if I miss a dose?
- Contact your doctor if you miss an appointment for your ibritumomab injection.
What happens if I overdose?
- Seek emergency medical attention if you think you have received too much of this medicine.
- Overdose symptoms may include weakness, pale skin, and easy bruising or bleeding.
What should I avoid while using ibritumomab?
- Avoid contact with people who have colds, the flu, or other contagious illnesses. Contact your doctor immediately if you develop signs of infection.
- Do not receive a "live" vaccine while you are being treated with ibritumomab, and avoid coming into contact with anyone who has recently received a live vaccine. There is a chance that the virus could be passed on to you.
How should it be stored?
- Keep out of the reach and sight of children.
- Do not use Ibritumomab after the expiry date which is stated on the pack.
- This medicine will be stored by a healthcare professional.
Store in a refrigerator (2°C - 8°C). Do not freeze. Store the vials in the original package in order to protect from light. Storage must be in accordance with national regulations for radioactive materials. - After radiolabelling, an immediate use is recommended. Stability has been demonstrated for 8 hours at 2°C - 8°C and protected from light.
Ibritumomab Tiuxetan
3.2mg/2ml Injection
INDICATIONS AND USAGE
Relapsed or Refractory, Low-grade or Follicular NHL
Ibritumomab Tiuxetan is indicated for the treatment of relapsed or refractory, low-grade or follicular B-cell non-Hodgkin's lymphoma (NHL).
Previously Untreated Follicular NHL
Ibritumomab Tiuxetan is indicated for the treatment of previously untreated follicular NHL in patients who achieve a partial or complete response to first-line chemotherapy.
DOSAGE AND ADMINISTRATION
Recommended Dosing Schedule:
- Administer the Ibritumomab Tiuxetan therapeutic regimen as outlined in Section 2.1.
- Initiate the Ibritumomab Tiuxetan therapeutic regimen following recovery of platelet counts to ≥150,000/mm3 at least 6 weeks, but no more than 12 weeks, following the last dose of first-line chemotherapy.
- Only administer Rituxan/Ibritumomab Tiuxetan in facilities where immediate access to resuscitative measures is available.
Overview of Dosing Schedule

Ibritumomab Tiuxetan Therapeutic Regimen Dosage and Administration
Day 1:
- Premedicate with acetaminophen 650 mg orally and diphenhydramine 50 mg orally prior to rituximab infusion.
- Administer rituximab 250 mg/m2 intravenously at an initial rate of 50 mg/hr. In the absence of infusion reactions, escalate the infusion rate in 50 mg/hr increments every 30 minutes to a maximum of 400 mg/hr. Do not mix or dilute rituximab with other drugs.
- Immediately stop the rituximab infusion for serious infusion reactions and discontinue the Ibritumomab Tiuxetan therapeutic regimen [see Boxed Warning and Warnings and Precautions (5.1)].
- Temporarily slow or interrupt the rituximab infusion for less severe infusion reactions. If symptoms improve, continue the infusion at one-half the previous rate.
Day 7, 8 or 9:
- Premedicate with acetaminophen 650 mg orally and diphenhydramine 50 mg orally prior to rituximab infusion.
- Administer rituximab 250 mg/m2 intravenously at an initial rate of 100 mg/hr. Increase rate by 100 mg/hr increments at 30 minute intervals, to a maximum of 400 mg/hr, as tolerated. If infusion reactions occurred during rituximab infusion on Day 1 of treatment, administer rituximab at an initial rate of 50 mg/hr and escalate the infusion rate in 50 mg/hr increments every 30 minutes to a maximum of 400 mg/hr.
- Administer Y-90 Ibritumomab Tiuxetan injection through a free flowing intravenous line within 4 hours following completion of rituximab infusion. Use a 0.22 micron low-protein-binding in-line filter between the syringe and the infusion port. After injection, flush the line with at least 10 mL of normal saline.
- If platelet count ≥ 150,000/mm3, administer Y-90 Ibritumomab Tiuxetan over 10 minutes as an intravenous injection at a dose of Y-90 0.4 mCi per kg (14.8 MBq per kg) actual body weight.
- If platelet count ≥ 100,000 but ≤ 149,000/mm3, in relapsed or refractory patients, administer Y-90 Ibritumomab Tiuxetan over 10 minutes as an intravenous injection at a dose of Y-90 0.3 mCi per kg (11.1 MBq per kg) actual body weight.
- Do not administer more than 32 mCi (1184 MBq) Y-90 Ibritumomab Tiuxetan dose regardless of the patient’s body weight.
- Monitor patients closely for evidence of extravasation during the injection of Y-90 Ibritumomab Tiuxetan. Immediately stop infusion and restart in another limb if any signs or symptoms of extravasation occur.
Directions for Preparation of Radiolabeled Y-90 Ibritumomab Tiuxetan Doses
A clearly-labeled kit is required for preparation of Yttrium-90 (Y-90) Ibritumomab Tiuxetan. Follow the detailed instructions for the preparation of radiolabeled Ibritumomab Tiuxetan.
Required materials not supplied in the kit:
- Yttrium-90 Chloride Sterile Solution
- Three sterile 1 mL plastic syringes
- One sterile 3 mL plastic syringe
- Two sterile 10 mL plastic syringes with 18-20 G needles
- ITLC silica gel strips
- 0.9% Sodium Chloride aqueous solution for the chromatography solvent
- Developing chamber for chromatography
- Suitable radioactivity counting apparatus
- Filter, 0.22 micrometer, low-protein-binding
- Appropriate acrylic shielding for reaction vial and syringe for Y-90
Method:
- Allow contents of the refrigerated Y-90 Ibritumomab Tiuxetan kit (Ibritumomab Tiuxetan vial, 50 mM sodium acetate vial, and formulation buffer vial) to reach room temperature.
- Place the empty reaction vial in an appropriate acrylic shield.
- Determine the amount of each component needed:
- Calculate volume of Y-90 Chloride equivalent to 40 mCi based on the activity concentration of the Y-90 Chloride stock.
- The volume of 50 mM Sodium Acetate solution needed is 1.2 times the volume of Y-90 Chloride solution determined in step 3.a, above.
- Calculate the volume of formulation buffer needed to bring the reaction vial contents to a final volume of 10 mL.
- Transfer the calculated volume of 50 mM Sodium Acetate to the empty reaction vial. Coat the entire inner surface of the reaction vial by gentle inversion or rolling.
- Transfer 40 mCi of Y-90 Chloride to the reaction vial using an acrylic shielded syringe. Mix the two solutions by gentle inversion or rolling.
- Transfer 1.3 mL of Ibritumomab Tiuxetan (ibritumomab tiuxetan) to the reaction vial. Do not shake or agitate the vial contents.
- Allow the labeling reaction to proceed at room temperature for 5 minutes. A shorter or longer reaction time may adversely alter the final labeled product.
- Immediately after the 5-minute incubation period, transfer the calculated volume of formulation buffer from step 3.c. to the reaction vial. Gently add the formulation buffer down the side of the reaction vial. If necessary, withdraw an equal volume of air to normalize pressure.
- Measure the final product for total activity using a radioactivity calibration system suitable for the measurement of Y-90.
- Using the supplied labels, record the date and time of preparation, the total activity and volume, and the date and time of expiration, and affix these labels to the shielded reaction vial container.
- Patient Dose: Calculate the volume required for a Y-90 Ibritumomab Tiuxetan dose. Withdraw the required volume from the reaction vial. Assay the syringe in the dose calibrator suitable for the measurement of Y-90. The measured dose must be within 10% of the prescribed dose of Y-90 Ibritumomab Tiuxetan and must not exceed 32 mCi (1184 MBq). Using the supplied labels, record the patient identifier, total activity and volume and the date and time of expiration, and affix these labels to the syringe and shielded unit dose container.
- Determine Radiochemical Purity.
- Store Yttrium-90 Ibritumomab Tiuxetan at 2-8°C (36-46°F) until use and administer within 8 hours of radiolabeling. Immediately prior to administration, assay the syringe and contents using a radioactivity calibration system suitable for the measurement of Y-90.
Procedure for Determining Radiochemical Purity
Use the following procedures for radiolabeling Y-90 Ibritumomab Tiuxetan:
- Place a small drop of Y-90 Ibritumomab Tiuxetan at the origin of an ITLC silica gel strip.
- Place the ITLC silica gel strip into a chromatography chamber with the origin at the bottom and the solvent front at the top. Allow the solvent (0.9% NaCl) to migrate at least 5 cm from the bottom of the strip. Remove the strip from the chamber and cut the strip in half. Count each half of the ITLC silica gel strip for one minute (CPM) with a suitable counting apparatus.
- Calculate the percent RCP as follows:

- Repeat the ITLC procedure if the radiochemical purity is <95%. If repeat testing confirms that radiochemical purity is <95%, do not administer the Y-90 Ibritumomab Tiuxetan dose.
Radiation Dosimetry
During clinical trials with Ibritumomab Tiuxetan, estimations of radiation-absorbed doses for Y-90 Ibritumomab Tiuxetan were performed using sequential whole body images and the MIRDOSE 3 software program. The estimated radiation absorbed doses to organs and marrow from a course of the Ibritumomab Tiuxetan therapeutic regimen are summarized in Table 1. Absorbed dose estimates for the lower large intestine, upper large intestine, and small intestine have been modified from the standard MIRDOSE 3 output to account for the assumption that activity is within the intestine wall rather than the intestine contents.
| Organ | Y-90 Ibritumomab Tiuxetan cGy /mCi (mGy/MBq) | |
|---|---|---|
| Median | Range | |
| Spleen* | 34.78 (9.4) | 6.66 - 74.00 (1.8 - 20.0) |
| Liver* | 17.76 (4.8) | 10.73 - 29.97 (2.9 - 8.1) |
| Lower Large Intestinal Wall* | 17.39 (4.7) | 11.47 - 30.34 (3.1 - 8.2) |
| Upper Large Intestinal Wall* | 13.32 (3.6) | 7.40 - 24.79 (2.0 - 6.7) |
| Heart Wall* | 10.73 (2.9) | 5.55 - 11.84 (1.5 - 3.2) |
| Lungs* | 7.4 (2) | 4.44 - 12.58 (1.2 -3.4) |
| Testes* | 5.55 (1.5) | 3.70 - 15.91 (1.0 - 4.3) |
| Small Intestine* | 5.18 (1.4) | 2.96 - 7.77 (0.8 - 2.1) |
| Red Marrow† | 4.81 (1.3) | 2.22 - 6.66 (0.6 - 1.8) |
| Urinary Bladder Wall‡ | 3.33 (0.9) | 2.59 - 4.81 (0.7 - 1.3) |
| Bone Surfaces† | 3.33 (0.9) | 1.85 - 4.44 (0.5 - 1.2) |
| Total Body‡ | 1.85 (0.5) | 1.48 - 2.59 (0.4 - 0.7) |
| Ovaries‡ | 1.48 (0.4) | 1.11 - 1.85 (0.3 - 0.5) |
| Uterus‡ | 1.48 (0.4) | 1.11 - 1.85 (0.3 - 0.5) |
| Adrenals‡ | 1.11 (0.3) | 0.74 - 1.85 (0.2 - 0.5) |
| Brain‡ | 1.11 (0.3) | 0.74 - 1.85 (0.2 - 0.5) |
| Breasts‡ | 1.11 (0.3) | 0.74 - 1.85 (0.2 - 0.5) |
| Gallbladder Wall‡ | 1.11 (0.3) | 0.74 - 1.85 (0.2 - 0.5) |
| Muscle‡ | 1.11 (0.3) | 0.74 - 1.85 (0.2 - 0.5) |
| Pancreas‡ | 1.11 (0.3) | 0.74 - 1.85 (0.2 - 0.5) |
| Skin‡ | 1.11 (0.3) | 0.74 - 1.85 (0.2 - 0.5) |
| Stomach‡ | 1.11 (0.3) | 0.74 - 1.85 (0.2 - 0.5) |
| Thymus‡ | 1.11 (0.3) | 0.74 - 1.85 (0.2 - 0.5) |
| Thyroid‡ | 1.11 (0.3) | 0.74 - 1.85 (0.2 - 0.5) |
| Kidneys* | 0.37 (0.1) | 0.00 - 1.11 (0.0 - 0.3) |
DOSAGE FORMS AND STRENGTHS
3.2 mg ibritumomab tiuxetan per 2 mL in a single-use vial.
CONTRAINDICATIONS
None.
WARNINGS AND PRECAUTIONS
Serious Infusion Reactions
See also prescribing information for rituximab.
Rituximab, alone or as a component of the Ibritumomab Tiuxetan therapeutic regimen, can cause severe, including fatal, infusion reactions. These reactions typically occur during the first rituximab infusion with time to onset of 30 to 120 minutes. Signs and symptoms of severe infusion reactions may include urticaria, hypotension, angioedema, hypoxia, bronchospasm, pulmonary infiltrates, acute respiratory distress syndrome, myocardial infarction, ventricular fibrillation, and cardiogenic shock. Temporarily slow or interrupt the rituximab infusion for less severe infusion reactions. Immediately discontinue rituximab and Y-90 Ibritumomab Tiuxetan administration for severe infusion reactions. Only administer Rituxan/Ibritumomab Tiuxetan in facilities where immediate access to resuscitative measures is available.
Prolonged and Severe Cytopenias
Cytopenias with delayed onset and prolonged duration, some complicated by hemorrhage and severe infection, are the most common severe adverse reactions of the Ibritumomab Tiuxetan therapeutic regimen. When used according to recommended doses, the incidences of severe thrombocytopenia and neutropenia are greater in patients with mild baseline thrombocytopenia (≥ 100,000 but ≤ 149,000 /mm3) compared to those with normal pretreatment platelet counts. Severe cytopenias persisting more than 12 weeks following administration can occur. Monitor complete blood counts (CBC) and platelet counts following the Ibritumomab Tiuxetan therapeutic regimen weekly until levels recover or as clinically indicated.
Do not administer the Ibritumomab Tiuxetan therapeutic regimen to patients with ≥ 25% lymphoma marrow involvement and/or impaired bone marrow reserve. Monitor patients for cytopenias and their complications (e.g., febrile neutropenia, hemorrhage) for up to 3 months after use of the Ibritumomab Tiuxetan therapeutic regimen. Avoid using drugs which interfere with platelet function or coagulation following the Ibritumomab Tiuxetan therapeutic regimen.
Severe Cutaneous and Mucocutaneous Reactions
Erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis, bullous dermatitis, and exfoliative dermatitis, some fatal, were reported in post-marketing experience. The time to onset of these reactions was variable, ranging from a few days to 4 months after administration of the Ibritumomab Tiuxetan therapeutic regimen. Discontinue the Ibritumomab Tiuxetan therapeutic regimen in patients experiencing a severe cutaneous or mucocutaneous reaction.
Altered Biodistribution
In a post-marketing registry designed to collect biodistribution images and other information in reported cases of altered biodistribution, there were 12 (1.3%) patients reported to have altered biodistribution among 953 patients registered.
Risk of Developing Myelodysplastic Syndrome, Leukemia, and Other Malignancies
The radiation dose resulting from therapeutic exposure to Y-90 radiolabeled Ibritumomab Tiuxetan may result in secondary malignancies.
Myelodysplastic syndrome (MDS) and/or acute myelogenous leukemia (AML) were reported in 5.2% (11/211) of patients with relapsed or refractory NHL enrolled in clinical studies and 1.5% (8/535) of patients included in the expanded-access trial, with median follow-up of 6.5 and 4.4 years, respectively. Among the 19 reported cases, the median time to the diagnosis of MDS or AML was 1.9 years following treatment with the Ibritumomab Tiuxetan therapeutic regimen; however, the cumulative incidence continues to increase.
Among 204 patients receiving Y-90 Ibritumomab Tiuxetan following first-line chemotherapy, 26 (12.7%) patients in the Ibritumomab Tiuxetan arm developed a second primary malignancy compared to 14 (6.8%) of patients in the control arm. Seven patients (3.4%, 7/204) were diagnosed with MDS/AML after receiving Ibritumomab Tiuxetan, compared to one patient (0.5%, 1/205) in the control arm, with a median follow-up of 7.3 years. Deaths due to second primary malignancy included 8 (3.9%) patients in the Ibritumomab Tiuxetan arm compared to 3 (1.5%) patients in the control arm. Deaths due to MDS/AML included five (2.5%) patients in the Ibritumomab Tiuxetan arm compared to no patients in the control arm.
Extravasation
Monitor patients closely for evidence of extravasation during Ibritumomab Tiuxetan infusion. Immediately terminate the infusion if signs or symptoms of extravasation occur and restart in another limb.
Risks of Immunization
The safety of immunization with live viral vaccines following the Ibritumomab Tiuxetan therapeutic regimen has not been studied. Do not administer live viral vaccines to patients who have recently received Ibritumomab Tiuxetan. The ability to generate an immune response to any vaccine following the Ibritumomab Tiuxetan therapeutic regimen has not been studied.
Radionuclide Precautions
During and after radiolabeling Ibritumomab Tiuxetan with Y-90, minimize radiation exposure to patients and to medical personnel, consistent with institutional good radiation safety practices and patient management procedures.
Embryo-Fetal Toxicity
Based on its radioactivity, Y-90 Ibritumomab Tiuxetan may cause fetal harm when administered to a pregnant woman. If the Ibritumomab Tiuxetan therapeutic regimen is administered during pregnancy, the patient should be apprised of the potential hazard to a fetus. Advise women of childbearing potential to use adequate contraception for a minimum of twelve months.
ADVERSE REACTIONS
The following serious adverse reactions are discussed in greater detail in other sections of the label:
- Serious Infusion Reactions [see Boxed Warning and Warnings and Precautions (5.1)].
- Prolonged and Severe Cytopenias [see Boxed Warning and Warnings and Precautions (5.2)].
- Severe Cutaneous and Mucocutaneous Reactions [see Boxed Warning and Warnings and Precautions (5.3)].
- Leukemia and Myelodysplastic Syndrome [see Warnings and Precautions (5.5)].
The most common adverse reactions of Ibritumomab Tiuxetan are cytopenias, fatigue, nasopharyngitis, nausea, abdominal pain, asthenia, cough, diarrhea, and pyrexia.
The most serious adverse reactions of Ibritumomab Tiuxetan are prolonged and severe cytopenias (thrombocytopenia, anemia, lymphopenia, neutropenia) and secondary malignancies.
Because the Ibritumomab Tiuxetan therapeutic regimen includes the use of rituximab, see prescribing information for rituximab.
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The reported safety data reflects exposure to Ibritumomab Tiuxetan in 349 patients with relapsed or refractory, low-grade, follicular or transformed NHL across 5 trials (4 single arm and 1 randomized) and in 206 patients with previously untreated follicular NHL in a randomized trial (Study 4) who received any portion of the Ibritumomab Tiuxetan therapeutic regimen. The safety data reflect exposure to Ibritumomab Tiuxetan in 270 patients with relapsed or refractory NHL with platelet counts ≥150,000/ mm3 who received 0.4 mCi/kg (14.8 MBq/kg) of Y-90 Ibritumomab Tiuxetan (Group 1 in Table 4), 65 patients with relapsed or refractory NHL with platelet counts of ≥ 100,000 but ≤ 149,000 /mm3 who received 0.3 mCi/kg (11.1 MBq/kg) of Y-90 Ibritumomab Tiuxetan (Group 2 in Table 4), and 204 patients with previously untreated NHL with platelet counts ≥150,000/ mm3 who received 0.4 mCi/kg (14.8 MBq/kg) of Y-90 Ibritumomab Tiuxetan; all patients received a single course of Ibritumomab Tiuxetan.
Table 2 displays selected adverse reaction incidence rates in patients who received any portion of the Ibritumomab Tiuxetan therapeutic regimen (n=206) or no further therapy (n=203) following first-line chemotherapy (Study 4).
| Ibritumomab Tiuxetan (n=206) | Observation (n=203) | |||
|---|---|---|---|---|
| All Grades† | Grade† 3-4 | All Grades† | Grade† 3-4 | |
| % | % | % | % | |
| Gastrointestinal Disorders | ||||
| Abdominal pain | 17 | 2 | 13 | <1 |
| Diarrhea | 11 | 0 | 3 | 0 |
| Nausea | 18 | 0 | 2 | 0 |
| Body as a Whole | ||||
| Asthenia | 15 | 1 | 8 | <1 |
| Fatigue | 33 | 1 | 9 | 0 |
| Influenza-like illness | 8 | 0 | 3 | 0 |
| Pyrexia | 10 | 3 | 4 | 0 |
| Musculoskeletal | ||||
| Myalgia | 9 | 0 | 3 | 0 |
| Metabolism | ||||
| Anorexia | 8 | 0 | 2 | 0 |
| Respiratory, Thoracic & Media | ||||
| Cough | 11 | <1 | 5 | 0 |
| Pharyngolaryngeal pain | 7 | 0 | 2 | 0 |
| Epistaxis | 5 | 2 | <1 | 0 |
| Nervous System | ||||
| Dizziness | 7 | 0 | 2 | 0 |
| Vascular | ||||
| Hypertension | 7 | 3 | 2 | <1 |
| Skin & Subcutaneous | ||||
| Night sweats | 8 | 0 | 2 | 0 |
| Petechiae | 8 | 2 | 0 | 0 |
| Pruritus | 7 | 0 | 1 | 0 |
| Rash | 7 | 0 | <1 | 0 |
| Infections & Infestations | ||||
| Bronchitis | 8 | 0 | 3 | 0 |
| Nasopharyngitis | 19 | 0 | 10 | 0 |
| Rhinitis | 8 | 0 | 2 | 0 |
| Sinusitis | 7 | <1 | <1 | 0 |
| Urinary tract infection | 7 | <1 | 3 | 0 |
| Blood and Lymphatic System | ||||
| Thrombocytopenia | 62 | 51 | 1 | 0 |
| Neutropenia | 45 | 41 | 3 | 2 |
| Anemia | 22 | 5 | 4 | 0 |
| Leukopenia | 43 | 36 | 4 | 1 |
| Lymphopenia | 26 | 18 | 9 | 5 |
Table 3 shows hematologic toxicities in 349 Ibritumomab Tiuxetan-treated patients with relapsed or refractory, low-grade, follicular or transformed B-cell NHL. Grade 2-4 hematologic toxicity occurred in 86% of Ibritumomab Tiuxetan-treated patients.
|
||
| All Grades % |
Grade 3-4 % |
|
|---|---|---|
| Thrombocytopenia | 95 | 63 |
| Neutropenia | 77 | 60 |
| Anemia | 61 | 17 |
| Ecchymosis | 7 | <1 |
Prolonged and Severe Cytopenias
Patients in clinical studies were not permitted to receive hematopoietic growth factors beginning 2 weeks prior to administration of the Ibritumomab Tiuxetan therapeutic regimen.
The incidence and duration of severe hematologic toxicity in previously treated NHL patients (N=335) and in previously untreated patients (Study 4) receiving Y-90 Ibritumomab Tiuxetan are shown in Table 4.
|
|||
| Baseline Platelet Count | Group 1 (n=270) ≥ 150,000/mm3 |
Group 2 (n=65 ) ≥ 100,000 but ≤ 149,000/mm3 |
Study 4 (n=204) ≥ 150,000/mm3 |
|---|---|---|---|
| Y-90 Ibritumomab Tiuxetan Dose | 0.4 mCi/kg (14.8 MBq/kg) |
0.3 mCi/kg (11.1 MBq/kg) | 0.4 mCi/kg (14.8 MBq/kg) |
| ANC | |||
| Median nadir ( per mm3) | 800 | 600 | 721 |
| Per Patient Incidence ANC <1000/mm3 | 57% | 74% | 65% |
| Per Patient Incidence ANC <500/mm3 | 30% | 35% | 26% |
| Median Duration (Days)* ANC <1000/mm3 | 22 | 29 | 29 |
| Median Time to Recovery† | 12 | 13 | 15 |
| Platelets | |||
| Median nadir (per mm3) | 41,000 | 24,000 | 42,000 |
| Per Patient Incidence Platelets <50,000/mm3 | 61% | 78% | 61% |
| Per Patient Incidence Platelets <10,000/mm3 | 10% | 14% | 4% |
| Median Duration (Days)‡ Platelets <50,000/mm3 | 24 | 35 | 26 |
| Median Time to Recovery† | 13 | 14 | 14 |
Cytopenias were more severe and more prolonged among eleven (5%) patients who received Ibritumomab Tiuxetan after first-line fludarabine or a fludarabine-containing chemotherapy regimen as compared to patients receiving non-fludarabine-containing regimens. Among these eleven patients, the median platelet nadir was 13,000/mm3 with a median duration of platelets below 50,000/mm3 of 56 days and the median time for platelet recovery from nadir to Grade 1 toxicity or baseline was 35 days. The median ANC was 355/mm3, with a median duration of ANC below 1,000/mm3 of 37 days and the median time for ANC recovery from nadir to Grade 1 toxicity or baseline was 20 days.
The median time to cytopenia was similar across patients with relapsed/refractory NHL and those completing first-line chemotherapy, with median ANC nadir at 61-62 days, platelet nadir at 49-53 days, and hemoglobin nadir at 68-69 days after Y-90-Ibritumomab Tiuxetan administration.
Information on hematopoietic growth factor use and platelet transfusions is based on 211 patients with relapsed/refractory NHL and 206 patients following first-line chemotherapy. Filgrastim was given to 13% of patients and erythropoietin to 8% with relapsed or refractory disease; 14% of patients receiving Ibritumomab Tiuxetan following first-line chemotherapy received granulocyte-colony stimulating factors and 5% received erythopoiesis-stimulating agents. Platelet transfusions were given to approximately 22% of all Ibritumomab Tiuxetan-treated patients. Red blood cell transfusions were given to 20% of patients with relapsed or refractory NHL and 2% of patients receiving Ibritumomab Tiuxetan following first-line chemotherapy.
Infections
In relapsed or refractory NHL patients, infections occurred in 29% of 349 patients during the first 3 months after initiating the Ibritumomab Tiuxetan therapeutic regimen and 3% developed serious infections (urinary tract infection, febrile neutropenia, sepsis, pneumonia, cellulitis, colitis, diarrhea, osteomyelitis, and upper respiratory tract infection). Life-threatening infections were reported in 2% (sepsis, empyema, pneumonia, febrile neutropenia, fever, and biliary stent-associated cholangitis). From 3 months to 4 years after Ibritumomab Tiuxetan treatment, 6% of patients developed infections; 2% were serious (urinary tract infection, bacterial or viral pneumonia, febrile neutropenia, perihilar infiltrate, pericarditis, and intravenous drug-associated viral hepatitis) and 1% were life-threatening infections (bacterial pneumonia, respiratory disease, and sepsis).
When administered following first-line chemotherapy (Table 2), Grade 3-4 infections occurred in 8% of Ibritumomab Tiuxetan treated patients and in 2% of controls and included neutropenic sepsis (1%), bronchitis, catheter sepsis, diverticulitis, herpes zoster, influenza, lower respiratory tract infection, sinusitis, and upper respiratory tract infection.
Leukemia and Myelodysplastic Syndrome
Among 746 patients with relapsed/refractory NHL, 19 (2.6%) patients developed MDS/AML with a median follow-up of 4.4 years. The overall incidence of MDS/AML among the 211 patients included in the clinical studies was 5.2% (11/211), with a median follow-up of 6.5 years and median time to development of MDS/AML of 2.9 years. The cumulative Kaplan-Meier estimated incidence of MDS/secondary leukemia in this patient population was 2.2% at 2 years and 5.9% at 5 years. The incidence of MDS/AML among the 535 patients in the expanded access programs was 1.5% (8/535) with a median follow-up of 4.4 years and median time to development of MDS/AML of 1.5 years. Multiple cytogenetic abnormalities were described, most commonly involving chromosomes 5 and/or 7. The risk of MDS/AML was not associated with the number of prior treatments (0-1 versus 2-10).
Among 204 patients receiving Y-90-Ibritumomab Tiuxetan following first-line treatment, 7 (3%) patients developed MDS/AML between approximately 2 and 7 years after Ibritumomab Tiuxetan administration.
Post-Marketing Experience
The following adverse reactions have been identified during post-approval use of the Ibritumomab Tiuxetan therapeutic regimen in hematologic malignancies. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Decisions to include these reactions in labeling are typically based on one or more of the following factors: (1) seriousness of the reaction, (2) frequency of reporting, or (3) strength of causal connection to the Ibritumomab Tiuxetan therapeutic regimen.
- Cutaneous and mucocutaneous reactions: erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis, bullous dermatitis, and exfoliative dermatitis.
- Infusion site erythema and ulceration following extravasation.
- Radiation injury in tissues near areas of lymphomatous involvement within a month of Ibritumomab Tiuxetan administration.
Immunogenicity
As with all therapeutic proteins, there is a potential for immunogenicity. The incidence of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparisons of the incidence of HAMA/HACA to the Ibritumomab Tiuxetan therapeutic regimen with the incidence of antibodies to other products may be misleading.
HAMA and HACA response data on 446 patients from 8 clinical studies conducted over a 10-year time period are available. Overall, 11/446 (2.5%) had evidence of either HAMA formation (N=8) or HACA formation (N=4). Six of these patients developed HAMA/HACA after treatment with Ibritumomab Tiuxetan and 5 were HAMA/HACA positive at baseline. Of the 6 who were HAMA/HACA positive, only one was positive for both. Furthermore, in 6 of the 11 patients, the HAMA/HACA reverted to negative within 2 weeks to 3 months. No patients had increasing levels of HAMA/HACA at the end of the studies.
Only 6/446 patients (1.3%) had developed evidence of antibody formation after treatment with Ibritumomab Tiuxetan, and of these, many either reverted to negative or decreased over time. This data demonstrates that HAMA/HACA develop infrequently, are typically transient, and do not increase with time.
DRUG INTERACTIONS
No formal drug interaction studies have been performed with Ibritumomab Tiuxetan. Patients receiving medications that interfere with platelet function or coagulation should have more frequent laboratory monitoring for thrombocytopenia.
USE IN SPECIFIC POPULATIONS
Pregnancy
Pregnancy Category D [see Warnings and Precautions]
Risk Summary
Based on its radioactivity, Y-90 Ibritumomab Tiuxetan may cause fetal harm when administered to a pregnant woman. Immunoglobulins are known to cross the placenta. There are no adequate and well-controlled studies in pregnant women. Animal reproductive toxicology studies of Ibritumomab Tiuxetan have not been conducted.
Advise women of childbearing potential to use adequate contraception for a minimum of twelve months. Inform women who become pregnant while receiving Ibritumomab Tiuxetan of the potential fetal risks.
Nursing Mothers
Because human IgG is excreted in human milk, it is expected that Ibritumomab Tiuxetan would be present in human milk. Because of the potential for adverse reactions in nursing infants from Y-90 Ibritumomab Tiuxetan, a decision should be made to discontinue nursing or not administer the Ibritumomab Tiuxetan therapeutic regimen, taking into account the importance of the drug to the mother.
Pediatric Use
The safety and effectiveness of Ibritumomab Tiuxetan have not been established in pediatric patients.
Geriatric Use
Of 349 patients with relapsed/refractory NHL treated with the Ibritumomab Tiuxetan therapeutic regimen in clinical studies, 38% (132 patients) were age 65 years and over, while 12% (41 patients) were age 75 years and over.
Of 414 patients enrolled in Study 4 (Ibritumomab Tiuxetan following first-line chemotherapy) 206 patients received Ibritumomab Tiuxetan. Of these patients 14% (29 patients) were 65 years and over, while 2% (4 patients) were 75 years and older. In the control arm, 10% (21 patients) were 65 years or over and 0% (0 patients) were 75 years or older.
No overall differences in safety or effectiveness were observed between these subjects and younger subjects, but greater sensitivity of some older individuals cannot be ruled out.
OVERDOSAGE
Severe cytopenias which may require stem cell support have occurred at doses higher than the recommended maximum total dose of 32 mCi (1184 MBq).
DESCRIPTION
Ibritumomab Tiuxetan (ibritumomab tiuxetan) is the immunoconjugate resulting from a stable thiourea covalent bond between the monoclonal antibody ibritumomab and the linker-chelator tiuxetan [N-[2-bis(carboxymethyl)amino]-3-(p-isothiocyanatophenyl)-propyl]-[N-[2-bis(carboxymethyl)amino]-2-(methyl)-ethyl]glycine. This linker-chelator provides a high affinity, conformationally restricted chelation site for Indium-111 or Yttrium-90. The approximate molecular weight of ibritumomab tiuxetan is 148 kD. The antibody moiety of Ibritumomab Tiuxetan is ibritumomab, a murine IgG1 kappa monoclonal antibody directed against the CD20 antigen.
Ibritumomab tiuxetan is a clear, colorless, sterile, pyrogen-free, preservative-free solution that may contain translucent particles. Each single-use vial includes 3.2 mg of ibritumomab tiuxetan in 2 mL of 0.9% Sodium Chloride.
Physical/Radiochemical Characteristics of Y-90
Yttrium-90 decays by emission of beta particles, with a physical half-life of 64.1 hours (2.67 days). The product of radioactive decay is non-radioactive Zirconium-90. The range of beta particles in soft tissue (χ90) is 5 mm. Radiation emission data for Y-90 are summarized in Table 5.
| Radiation | Mean % per Disintegration | Mean Energy (keV) |
|---|---|---|
| Beta minus | 100 | 750-935 |
External Radiation
The exposure rate for 1 mCi (37 MBq) of Y-90 is 8.3 x 10-3 C/kg/hr (32 R/hr) at the mouth of an open Y-90 vial.
To allow correction for physical decay of Y-90, the fractions that remain at selected intervals before and after the time of calibration are shown in Table 6.
| Calibration Time (Hrs.) | Fraction Remaining | Calibration Time (Hrs.) | Fraction Remaining |
|---|---|---|---|
| -36 | 1.48 | 0 | 1.00 |
| -24 | 1.30 | 1 | 0.99 |
| -12 | 1.14 | 2 | 0.98 |
| -8 | 1.09 | 3 | 0.97 |
| -7 | 1.08 | 4 | 0.96 |
| -6 | 1.07 | 5 | 0.95 |
| -5 | 1.06 | 6 | 0.94 |
| -4 | 1.04 | 7 | 0.93 |
| -3 | 1.03 | 8 | 0.92 |
| -2 | 1.02 | 12 | 0.88 |
| -1 | 1.01 | 24 | 0.77 |
| 0 | 1.00 | 36 | 0.68 |
CLINICAL PHARMACOLOGY
Mechanism of Action
Ibritumomab tiuxetan binds specifically to the CD20 antigen (human B-lymphocyte-restricted differentiation antigen, Bp35). The apparent affinity (KD) of ibritumomab tiuxetan for the CD20 antigen ranges between approximately 14 to 18 nM. The CD20 antigen is expressed on pre-B and mature B lymphocytes and on > 90% of B-cell non-Hodgkin’s lymphomas (NHL). The CD20 antigen is not shed from the cell surface and does not internalize upon antibody binding.
The chelate tiuxetan, which tightly binds Y-90, is covalently linked to ibritumomab. The beta emission from Y-90 induces cellular damage by the formation of free radicals in the target and neighboring cells.
Ibritumomab tiuxetan binding was observed in vitro on lymphoid cells of the bone marrow, lymph node, thymus, red and white pulp of the spleen, and lymphoid follicles of the tonsil, as well as lymphoid nodules of other organs such as the large and small intestines.
Pharmacodynamics
In clinical studies, administration of the Ibritumomab Tiuxetan therapeutic regimen resulted in sustained depletion of circulating B cells. At four weeks, the median number of circulating B cells was zero (range, 0-1084/mm3). B-cell recovery began at approximately 12 weeks following treatment, and the median level of B cells was within the normal range (32 to 341/mm3) by 9 months after treatment. Median serum levels of IgG and IgA remained within the normal range throughout the period of B-cell depletion. Median IgM serum levels dropped below normal (median 49 mg/dL, range 13-3990 mg/dL) after treatment and recovered to normal values by 6-months post therapy.
Pharmacokinetics
Pharmacokinetic and biodistribution studies were performed using In-111 Ibritumomab Tiuxetan (5 mCi [185 MBq] In-111, 1.6 mg ibritumomab tiuxetan). In an early study designed to assess the need for pre-administration of unlabeled antibody, only 18% of known sites of disease were imaged when In-111 Ibritumomab Tiuxetan was administered without unlabeled ibritumomab. When preceded by unlabeled ibritumomab (1.0 mg/kg or 2.5 mg/kg), In-111 Ibritumomab Tiuxetan detected 56% and 92% of known disease sites, respectively. These studies were conducted with a Ibritumomab Tiuxetan therapeutic regimen that included unlabeled ibritumomab.
In pharmacokinetic studies of patients receiving the Ibritumomab Tiuxetan therapeutic regimen, the mean effective half-life for Y-90 activity in blood was 30 hours, and the mean area under the fraction of injected activity (FIA) vs. time curve in blood was 39 hours. Over 7 days, a median of 7.2% of the injected activity was excreted in urine.
NONCLINICAL TOXICOLOGY
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity and mutogenicity studies have not been conducted. However, radiation is a potential carcinogen and mutagen.
No animal studies have been performed to determine the effects of Ibritumomab Tiuxetan on fertility in males or females. In clinical studies, the Ibritumomab Tiuxetan therapeutic regimen results in a significant radiation dose to the testes: the radiation dose to the ovaries has not been established. There is a potential risk that the Ibritumomab Tiuxetan therapeutic regimen could cause toxic effects on the male and female gonads. Effective contraceptive methods should be used during treatment and for up to 12 months following the Ibritumomab Tiuxetan therapeutic regimen.
Animal Toxicology and/or Pharmacology
Animal reproductive toxicology studies of the Ibritumomab Tiuxetan therapeutic regimen have not been conducted. Because the Ibritumomab Tiuxetan therapeutic regimen includes the use of rituximab, also see prescribing information for rituximab.
CLINICAL STUDIES
Relapsed or Refractory, Low-grade or Follicular Lymphoma
Study 1 was a single arm study of 54 patients with relapsed follicular lymphoma, who were refractory to rituximab treatment. Patients had a World Health Organization (WHO) Performance Status (PS) 0-2, <25% bone marrow involvement by NHL, no prior bone marrow transplantation, and acceptable hematologic, renal, and hepatic function. Refractoriness to rituximab was defined as failure to achieve a complete or partial response or time-to-disease-progression (TTP) of < 6 months. The main efficacy outcome measure of the study was the overall response rate (ORR) using the International Workshop Response Criteria (IWRC). Other efficacy outcome measures included time-to-disease-progression (TTP) and duration of response (DR). Table 7 summarizes efficacy data from Study 1.
Study 2 was a randomized (1:1), open-label, multicenter study comparing the Ibritumomab Tiuxetan therapeutic regimen with rituximab. The trial was conducted in 130 patients with relapsed or refractory low-grade or follicular non-Hodgkin's lymphoma (NHL); no patient had received prior rituximab. Patients had histologically confirmed NHL requiring therapy, a WHO PS 0-2, <25% bone marrow involvement by NHL, no prior bone marrow transplantation, and acceptable hematologic function. Sixty-four patients received the Ibritumomab Tiuxetan therapeutic regimen, and 66 patients received rituximab given as an IV infusion at 375 mg per m2 weekly times 4 doses. The main efficacy outcome measure of the study was ORR using the IWRC. The ORR was significantly higher for patients receiving the Ibritumomab Tiuxetan therapeutic regimen (83% vs. 55%, p<0.001). Time-to-disease-progression was not significantly different between study arms. Table 7 summarizes efficacy data from Study 2.
|
|||
| Study 1 | Study 2 | ||
|---|---|---|---|
| Ibritumomab Tiuxetan therapeutic regimen N = 54 |
Ibritumomab Tiuxetan therapeutic regimen N = 64 |
Rituximab N = 66 |
|
| Overall Response Rate (%) | 74 | 83 | 55 |
| Complete Response Rate† (%) | 15 | 38 | 18 |
|
(Months) [Range¶] | 6.4 [0.5-49.9+] | 14.3 [1.8-47.6+] | 11.5 [1.2-49.7+] |
| Median TTP‡,#(Months) [Range¶] | 6.8 [1.1-50.9+] | 12.1 [2.1-49.0+] | 10.1 [0.7-51.3+] |
Study 3 was a single arm study of 30 patients of whom 27 had relapsed or refractory low-grade, follicular NHL and a platelet count 100,000 to 149,000/mm3. Patients with ≥ 25% lymphomatous marrow involvement, prior myeloablative therapy with stem cell support, prior external beam radiation to > 25% of active marrow or neutrophil count <1,500/mm3 were ineligible for Study 3. All patients received Y-90 Ibritumomab Tiuxetan [0.3 mCi per kg (11.1 MBq per kg)]. Objective, durable clinical responses were observed [89% ORR (95% CI: 70-97%) with a median duration of response of 11.6 months (range: 1.0-42.4+ months)].
Follicular, B-Cell NHL Upon Completion of First-Line Chemotherapy
Study 4 was a multi-center, randomized, open-label study conducted in patients with follicular NHL with a partial (PR) or complete response (CR/CRu) upon completion of first-line chemotherapy. Randomization was stratified by center and response to first-line therapy (CR or PR). Key eligibility criteria were <25% bone marrow involvement, no prior external beam radiation or myeloablative therapy, and recovery of platelets to normal levels. Patients were randomized to receive Ibritumomab Tiuxetan (n=208) or no further therapy (n=206). Y-90 Ibritumomab Tiuxetan was administered at least 6 weeks but no more than 12 weeks following the last dose of chemotherapy. The main efficacy outcome measure was progression-free survival (PFS) assessed by study investigators using the International Workshop to Standardize Response Criteria for non-Hodgkin’s Lymphoma (1999).
Among the 414 patients, 49% were male, 99% were Caucasian, 12% were ≥65 years old, 83% had a WHO performance status of 0, and 65% had Stage IV disease. Thirty-nine (9.5%) patients received single agent chlorambucil, 22 (5%) patients received fludarabine or a fludarabine-containing regimen, 294 (71%) patients received cyclophosphamide-containing combination chemotherapy [CHOP (31%); CHOP-like (15%); CVP/COP (26%)] and 59 (14%) patients received rituximab-containing combination chemotherapy as first-line treatment.
Progression-free survival was significantly prolonged among Ibritumomab Tiuxetan-treated patients compared to those receiving no further treatment [median PFS 38 months vs. 18 months; HR 0.46 (95% CI: 0.35, 0.60) p<0.0001 Cox model stratified by response to first-line therapy and initial treatment strategy (immediate vs. watch-and-wait)]. The number of patients who died was too small to permit a reliable comparison on survival.
The results for PFS are presented in Figure 1.
Figure 1. Study 4: Kaplan-Meier Estimator for Investigator-Assessed Progression Free Survival Time

HOW SUPPLIED/STORAGE AND HANDLING
A kit is used for preparing Y-90 radiolabeled Ibritumomab Tiuxetan (NDC 68152-103-03). The contents of all vials are sterile, pyrogen-free, contain no preservatives, and are not radioactive. The kit contains four identification labels and the following four vials:
- One (1) Ibritumomab Tiuxetan vial containing 3.2 mg ibritumomab tiuxetan in 2 mL 0.9% Sodium Chloride as a clear, colorless solution.
- One (1) 50 mM Sodium Acetate Vial containing 13.6 mg Sodium Acetate trihydrate in 2 mL Water for Injection, USP as a clear, colorless solution.
- One (1) Formulation Buffer Vial containing 750 mg Albumin (Human), 76 mg Sodium Chloride, 28 mg Sodium Phosphate Dibasic Dodecahydrate, 4 mg Pentetic Acid, 2 mg Potassium Phosphate Monobasic and 2 mg Potassium Chloride in 10 mL Water for Injection, pH 7.1 as a clear yellow to amber colored solution.
- One (1) empty Reaction Vial.
Yttrium-90 Chloride Sterile Solution is shipped directly from the supplier upon placement of an order for the Y-90 Ibritumomab Tiuxetan kit.
Storage
Store the kit at 2-8°C (36-46°F). Do not freeze.
PATIENT COUNSELING INFORMATION
Advise patients:
- To contact a healthcare professional for severe signs and symptoms of infusion reactions
- To take premedications as prescribed [see Dosage and Administration (2.2) and Warnings and Precautions (5.1)].
- To report any signs or symptoms of cytopenias (bleeding, easy bruising, petechiae or purpura, pallor, weakness or fatigue) [see Warnings and Precautions (5.2)].
- To avoid medications that interfere with platelet function, except as directed by a healthcare professional [see Warnings and Precautions (5.2)].
- To seek prompt medical evaluation for diffuse rash, bullae, or desquamation of the skin or oral mucosa [see Warnings and Precautions (5.3)].
- To immediately report symptoms of infection (e.g. pyrexia) [see Adverse Reactions (6.2)].
- That immunization with live viral vaccines is not recommended for 12 months following the Ibritumomab Tiuxetan therapeutic regimen [see Warnings and Precautions (5.7)].
- To use effective contraceptive methods during treatment and for a minimum of 12 months following Ibritumomab Tiuxetan therapy [see Warnings and Precautions (5.9)], Use in Specific Populations (8.1)and Nonclinical Toxicology (13.1)].
- To discontinue nursing during and after Ibritumomab Tiuxetan treatment [see Use In SpecificPopulations (8.3)].
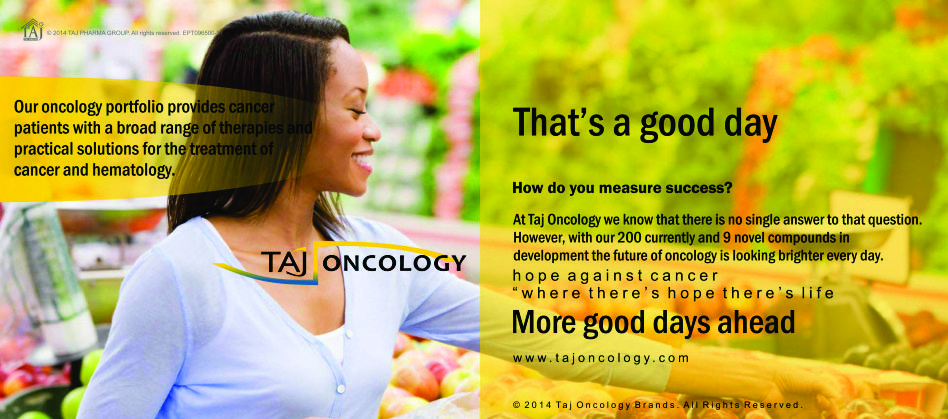
Product Glimpse
Description
We are committed to work towards a healthier and happier world. The company is an integrated, research based international pharmaceutical company, producing a wide range of quality, affordable generic (Ibritumomab tiuxetan 3.2mg/2ml Injection) medicines, trusted by health-care professionals and patients across geographies.
We offer you the highest quality new Generic medicines ie. Ibritumomab tiuxetan 3.2mg/2ml Injection, drugs and also with innovative packing at the lowest prices shipped to you from India. Browse our latest Pharmaceuticals and Generics possibilities and other pharmaceuticals possibilities…more.