Ibandronate sodium 150mg Tablets
Ibandronate sodium
150mg Tablets
Ibandronate sodium tablets, 150 mg (ibandronate): supplied as white to off-white, capsule-shaped tablets with “IN 150” on one side and ℑ on the other side and packaged in:
Carton of 3 blister packs, each blister containing 1 tablet
Store at 20°C - 25°C (68°F - 77°F) [See USP Controlled Room Temperature].
Ibandronate sodium is available as a white to off-white, capsule-shaped 150-mg tablet for once-monthly oral administration. One 150-mg tablet contains 168.75 mg ibandronate monosodium monohydrate, equivalent to 150 mg free acid. Ibandronate sodium tablets also contain the following inactive ingredients: sorbitol, microcrystalline cellulose, colloidal anhydrous silica, croscarmellose sodium, sodium stearyl fumarate and Ibandronate sodium- II white
Ibandronate sodium tablets are indicated for the treatment and prevention of osteoporosis in postmenopausal women. Ibandronate sodium tablets increase bone mineral density (BMD) and reduce the incidence of vertebral fractures.
The optimal duration of use has not been determined. The safety and effectiveness of ibandronate sodium tablets for the treatment of osteoporosis are based on clinical data of three years duration. All patients on bisphosphonate therapy should have the need for continued therapy re-evaluated on a periodic basis. Patients at low-risk for fracture should be considered for drug discontinuation after 3 to 5 years of use. Patients who discontinue therapy should have their risk for fracture re-evaluated periodically.
Ibandronate sodium
150mg Tablets
WHAT IBANDRONIC ACID IS AND WHAT IT IS USED FOR
The name of your medicine is Ibandronic acid 150mg film-coated Tablets (referred to as ibandronic acid throughout this leaflet).
Ibandronic acid belongs to a group of medicines called bisphosphonates. It contains Ibandronic acid. It does not contain hormones.
Ibandronic acid may reverse bone loss by stopping more loss of bone and increasing bone mass in most women who take it, even though they won't be able to see or feel a difference. Ibandronic acid may help lower the chances of breaking bones (fractures). This reduction in fractures was shown for the spine but not the hip.
Ibandronic acid is prescribed to you to treat postmenopausal osteoporosis because you have an increased risk of fractures. Osteoporosis is thinning and weakening of the bones, which is common in women after the menopause. At the menopause, a woman's ovaries stop producing the female hormone, oestrogen, which helps to keep skeleton healthy.
The earlier a woman reaches the menopause, the greater the risk of fractures in osteoporosis. Other things that can increase the risk of fractures include:
- not enough calcium and vitamin D in the diet
- smoking, or drinking too much alcohol
- not enough walking or other weight-bearing exercise
- a family history of osteoporosis.
Many people with osteoporosis have no symptoms. If you have no symptoms you may not know if you have the condition. However, osteoporosis makes you more likely to break bones if you fall or hurt yourself. A broken bone after the age of 50 may be a sign of osteoporosis. Osteoporosis can also cause back pain, height loss and a curved back.
Ibandronic acid prevents loss of bone from osteoporosis, and helps to rebuild bone. Therefore Ibandronic acid makes bone less likely to break.
A healthy lifestyle will also help you to get the most benefit from your treatment. This includes eating a balanced diet rich in calcium and vitamin D; walking or any other weight-bearing exercise; not smoking and not drinking too much alcohol.
BEFORE YOU USE IBANDRONIC ACID
Do not use Ibandronic acid
- If you are allergic (hypersensitive) to Ibandronic acid, or to any of the other ingredients of Ibandronic acid 150mg film-coated tablets.
- If you have certain problems with your oesophagus (the tube connecting your mouth with your stomach) such as narrowing or difficulty swallowing.
- If you can't stand or sit upright for at least one hour (60 minutes) at a time.
- If you have, or had in the past low blood calcium.
Please consult your doctor.
Children and teenagers
Do not give Ibandronic acid to children or teenagers.
Take special care with Ibandronic acid
Some people need to be especially careful while they're taking Ibandronic acid. Check with your doctor:
- If you have any disturbances of mineral metabolism (such as vitamin D deficiency).
- If your kidneys are not functioning normally.
- If you have any swallowing or digestive problems.
- If you are under dental treatment or will undergo dental surgery, tell your dentist that you are being treated with Ibandronic acid.
Irritation, inflammation or ulceration of the oesophagus (the tube connecting your mouth with your stomach) often with symptoms of severe pain in the chest, severe pain after swallowing food and/or drink, severe nausea, or vomiting may occur, especially if you do not drink a full glass of plain water and/or if you lie down within an hour of taking Ibandronic acid . If you develop these symptoms, stop taking Ibandronic acid and tell your doctor straight away.
Taking other medicines
Please tell your doctor or pharmacist if you are taking, or have recently taken any other medicines, including medicines obtained without prescription. Especially:
- Supplements containing calcium, magnesium, iron or aluminum, as they could possibly influence the effects of Ibandronic acid.
- Aspirin and other non-steroidal anti-inflammatory medicines (NSAIDs) ( including ibuprofen, diclofenac sodium and naproxen) may irritate the stomach and intestine. Bisphosphonates (like Ibandronic acid) may also do so. So be especially careful if you take painkillers or anti-inflammatories while you're taking Ibandronic acid.
After swallowing your monthly Ibandronic acid tablet, wait for 1 hour before taking any other medication, including indigestion tablets, calcium supplements, or vitamins.
Taking Ibandronic acid with food and drinks
Do not take Ibandronic acid with food. Ibandronic acid is less effective if it's taken with food.
You can drink plain water but no other drinks (see 3. HOW TO TAKE IBANDRONIC ACID).
Pregnancy and breast-feeding
Do not take Ibandronic acid if you're pregnant or breast feeding. If you're breast feeding, you may need to stop in order to take Ibandronic acid.
Ask your doctor or pharmacist for advice before taking any medicines.
Driving and using machines
You can drive and use machines as it's very unlikely that Ibandronic acid will affect your ability to drive and use machines.
Important information about some of the ingredients of Ibandronic acid
The product contains lactose. If you have been told by your doctor that you have an intolerance to some sugars, contact your doctor before taking this medicinal product.
HOW TO USE IBANDRONIC ACID
Always take Ibandronic acid exactly as your doctor has told you. If you're not sure about anything, ask your doctor or pharmacist.
The Usual Dose Of Ibandronic Acid Is One Tablet Once A Month.
Taking your monthly tablet
It's important to follow these instructions carefully. They are designed to help your Ibandronic acid tablet reach your stomach quickly, so it's less likely to cause irritation.
- Take one Ibandronic acid 150 mg tablet once a month.
- Choose one day of the month that will be easy to remember. You can choose either the same date (such as the 1st of each month) or the same day (such as the first Sunday of each month) to take your Ibandronic acid tablet. Choose the date that fits your routine.
- Take your Ibandronic acid tablet at least 6 hours after you last had anything to eat or drink except plain water.
- Take your Ibandronic acid tablet:
- after you first get up for the day, and
- before you have anything to eat or drink (on an empty stomach)
- Swallow your tablet with a full glass of plain water (at least 180 ml). Do not take your tablet with mineral water, fruit juice or any other drinks.
- Swallow your tablet whole - do not chew it, crush it or let it dissolve in your mouth.
- For the next hour (60 minutes) after you've taken your tablet
- do not lie down; if you do not stay upright (standing or sitting), some of the medicine could leak back into your oesophagus
- do not eat anything
- do not drink anything (except plain water if you need it)
- do not take any other medicines
- After you've waited for an hour, you can have your first food and drink of the day. Once you've eaten, it's OK to lie down if you wish, and to take any other medication you need.
Do not take your tablet at bedtime or before you get up for the day.
Continuing to take Ibandronic acid
It's important to keep taking Ibandronic acid every month, as long as your doctor prescribes it for you. Ibandronic acid can treat osteoporosis only as long as you keep taking it.
If you take too much Ibandronic acid
If you've taken more than one tablet by mistake, drink a full glass of milk and talk to your doctor straight away.
Do not make yourself vomit, and do not lie down - this could cause Ibandronic acid to irritate your oesophagus.
If you forget a dose
If you forget to take your tablet on the morning of your chosen day, do not take a tablet later in the day.
Instead, consult your calendar and find out when your next scheduled dose is:
- If your next scheduled dose is only 1 to 7 days away...
You should wait until the next scheduled close is due and take it as normal; then, continue taking one tablet once a month on the scheduled days you've marked on your calendar. - If your next scheduled dose is more than 7 days away..
You should take one tablet the next morning after the day you remember; then, continue taking one tablet once a month on the scheduled days you've marked on your calendar.
Never take two Ibandronic acid tablets within the same week.
POSSIBLE SIDE EFFECTS
Like all medicines, Ibandronic acid can cause side effects, although not everybody gets them.
Talk to a nurse or a doctor straight away if you notice any of the following serious side effects - you may need urgent medical treatment:
- rash, itching, swelling of your face, lips, tongue and throat, with difficulty breathing. You may be having an allergic reaction to the medicine.
- severe pain in the chest, severe pain after swallowing food or drink, severe nausea, or vomiting.
- flu-like symptoms (if any effects become troublesome or last more than a couple of days).
- pain or sore in your mouth or jaw
- eye pain and inflammation (if prolonged)
Other possible effects
Common (affect less than 1 in 10 people)
- headache
- heartburn, stomach pain (such as "gastroenteritis" or "gastritis"), indigestion, nausea, having diarrhoea or constipation
- rash
- pain or stiffness in your muscles, joints, or back
- flu-like symptoms (including fever, shaking and shivering, feeling of discomfort, fatigue, bone pain and aching muscles and joints)
- fatigue
Uncommon (affects less than 1 in 100 people)
- bone pain
- feeling weak
- dizziness,
- flatulence.
Rare (affects less than 1 in 1000 people):
- hypersensitivity reaction; swelling of the face, lips and mouth (see allergy)
- itching
- eye pain or inflammation
- unusual fracture of the thigh bone particularly in patients on long-term treatment for osteoporosis may occur rarely. Contact your doctor if you experience pain, weakness or discomfort in your thigh, hip or groin as this may be an early indication of possible fracture of the thigh bone.
Very rare (affect less than 1 in 10000 people)
- a condition involving exposed bone in the mouth called "osteonecrosis of the jaw".
If any of the side effects gets serious or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist
HOW TO STORE IBANDRONIC ACID
Keep out of the reach and sight of children.
This medicinal product does not require any special storage conditions.
Do not use after the expiry date which is stated on the carton after "EXP". The expiry date refers to the last day of the month.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. These measures will help to protect environment.
FURTHER INFORMATION
What Ibandronic acid contains
- The active substance is ibandronic acid. One tablet contains 150mg of ibandronic acid.
- The other ingredients are:
Core: Lactose, Povidone, Crospovidone, Magnesium Stearate.
Coating: Mixture of, Polyethylene glycol, Titanium Dioxide, Talc and Polyvinyl alcohol
What Ibandronic acid 150mg Tablets looks like and content of the pack
Ibandronic acid 150mg Tablets are white, oblong biconvex film coated tablets.
Pack sizes:
10, 20 or 30 film-coated tablets
Not all pack sizes may be marketed
Ibandronate sodium
150mg Tablets
INDICATIONS AND USAGE
Treatment and Prevention of Postmenopausal Osteoporosis
Ibandronate sodium tablets are indicated for the treatment and prevention of osteoporosis in postmenopausal women. Ibandronate sodium tablets increase bone mineral density (BMD) and reduce the incidence of vertebral fractures.
Important Limitations of Use
The optimal duration of use has not been determined. The safety and effectiveness of ibandronate sodium tablets for the treatment of osteoporosis are based on clinical data of three years duration. All patients on bisphosphonate therapy should have the need for continued therapy re-evaluated on a periodic basis. Patients at low-risk for fracture should be considered for drug discontinuation after 3 to 5 years of use. Patients who discontinue therapy should have their risk for fracture re-evaluated periodically.
DOSAGE AND ADMINISTRATION
Dosage Information
The dose of ibandronate sodium is one 150 mg tablet taken once monthly on the same date each month.
Important Administration Instructions
Instruct Patients to do the following:
- Take ibandronate sodium tablets at least 60 minutes before the first food or drink (other than water) of the day or before taking any oral medication or supplementation, including calcium, antacids, or vitamins to maximize absorption and clinical benefit. Avoid the use of water with supplements including mineral water because they may have a higher concentration of calcium.
- Swallow ibandronate sodium tablets whole with a full glass of plain water (6 to 8 oz) while standing or sitting in an upright position to reduce the potential for esophageal irritation. Avoid lying down for 60 minutes after taking ibandronate sodium tablets. Do not chew or suck the tablet because of a potential for oropharyngeal ulceration.
- Do not eat, drink anything except plain water, or take other medications for at least 60 minutes after taking ibandronate sodium tablets.
Recommendations for Calcium and Vitamin D Supplementation
Instruct patients to take supplemental calcium and vitamin D if their dietary intake is inadequate. Avoid the use of calcium supplements within 60 minutes of ibandronate sodium tablets administration because coadministration of ibandronate sodium tablets and calcium may interfere with the absorption of ibandronate sodium.
Administration Instructions for Missed Once-Monthly Doses
If the once-monthly dose is missed, instruct patients to do the following:
- If the next scheduled ibandronate sodium tablets day is more than 7 days away, take one ibandronate sodium 150 mg tablet in the morning following the date that it is remembered.
- If the next scheduled ibandronate sodium tablets day is only 1 to 7 days away, wait until the subsequent month’s scheduled ibandronate sodium tablets day to take their tablet.
For subsequent monthly doses for both of the above scenarios, instruct patients to return to their original schedule by taking one ibandronate sodium 150 mg tablet every month on their previous chosen day.
DOSAGE FORMS AND STRENGTHS
Tablets: 150 mg
CONTRAINDICATIONS
Ibandronate sodium tablets are contraindicated in patients with the following conditions:
- Abnormalities of the esophagus which delay esophageal emptying such as stricture or achalasia
- Inability to stand or sit upright for at least 60 minutes
- Hypocalcemia
- Known hypersensitivity to ibandronate sodium tablets or to any of its excipients. Cases of anaphylaxis have been reported
WARNINGS AND PRECAUTIONS
Upper Gastrointestinal Adverse Reactions
Ibandronate sodium, like other bisphosphonates administered orally, may cause local irritation of the upper gastrointestinal mucosa. Because of these possible irritant effects and a potential for worsening of the underlying disease, caution should be used when ibandronate sodium is given to patients with active upper gastrointestinal problems (such as known Barrett’s esophagus, dysphagia, other esophageal diseases, gastritis, duodenitis or ulcers).
Esophageal adverse experiences, such as esophagitis, esophageal ulcers and esophageal erosions, occasionally with bleeding and rarely followed by esophageal stricture or perforation, have been reported in patients receiving treatment with oral bisphosphonates. In some cases, these have been severe and required hospitalization. Physicians should therefore be alert to any signs or symptoms signaling a possible esophageal reaction and patients should be instructed to discontinue ibandronate sodium and seek medical attention if they develop dysphagia, odynophagia, retrosternal pain or new or worsening heartburn.
The risk of severe esophageal adverse experiences appears to be greater in patients who lie down after taking oral bisphosphonates and/or who fail to swallow it with the recommended full glass (6 to 8 oz) of water, and/or who continue to take oral bisphosphonates after developing symptoms suggestive of esophageal irritation. Therefore, it is very important that the full dosing instructions are provided to, and understood by, the patient. In patients who cannot comply with dosing instructions due to mental disability, therapy with ibandronate sodium should be used under appropriate supervision.
There have been postmarketing reports of gastric and duodenal ulcers with oral bisphosphonate use, some severe and with complications, although no increased risk was observed in controlled clinical trials.
Hypocalcemia and Mineral Metabolism
Hypocalcemia has been reported in patients taking ibandronate sodium. Treat hypocalcemia and other disturbances of bone and mineral metabolism before starting ibandronate sodium therapy. Instruct patients to take supplemental calcium and vitamin D if their dietary intake is inadequate.
Musculoskeletal Pain
Severe and occasionally incapacitating bone, joint, and/or muscle pain has been reported in patients taking ibandronate sodium and other bisphosphonates. The time to onset of symptoms varied from one day to several months after starting the drug. Most patients had relief of symptoms after stopping. A subset had recurrence of symptoms when rechallenged with the same drug or another bisphosphonate. Consider discontinuing use if severe symptoms develop.
Jaw Osteonecrosis
Osteonecrosis of the jaw (ONJ), which can occur spontaneously, is generally associated with tooth extraction and/or local infection with delayed healing, and has been reported in patients taking bisphosphonates, including ibandronate sodium. Known risk factors for osteonecrosis of the jaw include invasive dental procedures (e.g., tooth extraction, dental implants, boney surgery), diagnosis of cancer, concomitant therapies (e.g., chemotherapy, corticosteroids), poor oral hygiene, and co-morbid disorders (e.g., periodontal and/or other pre-existing dental disease, anemia, coagulopathy, infection, ill-fitting dentures). The risk of ONJ may increase with duration of exposure to bisphosphonates.
For patients requiring invasive dental procedures, discontinuation of bisphosphonate treatment may reduce the risk for ONJ. Clinical judgment of the treating physician and/or oral surgeon should guide the management plan of each patient based on individual benefit/risk assessment.
Patients who develop osteonecrosis of the jaw while on bisphosphonate therapy should receive care by an oral surgeon. In these patients, extensive dental surgery to treat ONJ may exacerbate the condition. Discontinuation of bisphosphonate therapy should be considered based on individual benefit/risk assessment.
Atypical Subtrochanteric and Diaphyseal Femoral Fractures
Atypical, low-energy, or low-trauma fractures of the femoral shaft have been reported in bisphosphonate-treated patients. These fractures can occur anywhere in the femoral shaft from just below the lesser trochanter to above the supracondylar flare and are transverse or short oblique in orientation without evidence of comminution. Causality has not been established as these fractures also occur in osteoporotic patients who have not been treated with bisphosphonates.
Atypical femur fractures most commonly occur with minimal or no trauma to the affected area. They may be bilateral and many patients report prodromal pain in the affected area, usually presenting as dull, aching thigh pain, weeks to months before a complete fracture occurs. A number of reports note that patients were also receiving treatment with glucocorticoids (e.g., prednisone) at the time of fracture.
Any patient with a history of bisphosphonate exposure who presents with thigh or groin pain should be suspected of having an atypical fracture and should be evaluated to rule out an incomplete femur fracture. Patients presenting with an atypical fracture should also be assessed for symptoms and signs of fracture in the contralateral limb. Interruption of bisphosphonate therapy should be considered, pending a risk/benefit assessment, on an individual basis.
Severe Renal Impairment
Ibandronate sodium is not recommended for use in patients with severe renal impairment (creatinine clearance of less than 30 mL/min).
ADVERSE REACTIONS
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Treatment and Prevention of Postmenopausal Osteoporosis
Daily Dosing
The safety of ibandronate sodium 2.5 mg once daily in the treatment and prevention of postmenopausal osteoporosis was assessed in 3577 patients aged 41 to 82 years. The duration of the trials was 2 to 3 years, with 1134 patients exposed to placebo and 1140 exposed to ibandronate sodium 2.5 mg. Patients with pre-existing gastrointestinal disease and concomitant use of non-steroidal anti-inflammatory drugs, proton pump inhibitors and H2 antagonists were included in these clinical trials. All patients received 500 mg calcium plus 400 international units vitamin D supplementation daily.
The incidence of all-cause mortality was 1% in the placebo group and 1.2% in the ibandronate sodium 2.5 mg daily group. The incidence of serious adverse reactions was 20% in the placebo group and 23% in the ibandronate sodium 2.5 mg daily group. The percentage of patients who withdrew from treatment due to adverse reactions was approximately 17% in both the ibandronate sodium 2.5 mg daily group and the placebo group. Table 1 lists adverse reactions from the treatment and prevention studies reported in greater than or equal to 2% of patients and more frequently in patients treated daily with ibandronate sodium than patients treated with placebo.
| Body System | Placebo % (n=1134) |
Ibandronate Sodium 2.5 mg % (n=1140) |
|---|---|---|
| Body as a Whole | ||
| Back Pain | 12 | 14 |
| Pain in Extremity | 6 | 8 |
| Asthenia | 2 | 4 |
| Allergic Reaction | 2 | 3 |
| Digestive System | ||
| Dyspepsia | 10 | 12 |
| Diarrhea | 5 | 7 |
| Tooth Disorder | 2 | 4 |
| Vomiting | 2 | 3 |
| Gastritis | 2 | 2 |
| Musculoskeletal System | ||
| Myalgia | 5 | 6 |
| Joint Disorder | 3 | 4 |
| Arthritis | 3 | 3 |
| Nervous System | ||
| Headache | 6 | 7 |
| Dizziness | 3 | 4 |
| Vertigo | 3 | 3 |
| Respiratory System | ||
| Upper Respiratory Infection | 33 | 34 |
| Bronchitis | 7 | 10 |
| Pneumonia | 4 | 6 |
| Pharyngitis | 2 | 3 |
| Urogenital System | 4 | 6 |
| Urinary Tract Infection | 4 | 6 |
Gastrointestinal Adverse Reactions
The incidence of selected gastrointestinal adverse reactions in the placebo and ibandronate sodium 2.5 mg daily groups were: dyspepsia (10% vs. 12%), diarrhea (5% vs. 7%), and abdominal pain (5% vs. 6%).
Musculoskeletal Adverse Reactions
The incidence of selected musculoskeletal adverse reactions in the placebo and ibandronate sodium 2.5 mg daily groups were: back pain (12% vs. 14%), arthralgia (14% vs. 14%) and myalgia (5% vs. 6%).
Ocular Adverse Events
Reports in the medical literature indicate that bisphosphonates may be associated with ocular inflammation such as iritis and scleritis. In some cases, these events did not resolve until the bisphosphonate was discontinued. There were no reports of ocular inflammation in studies with ibandronate sodium 2.5 mg daily.
Monthly Dosing
The safety of ibandronate sodium 150 mg once monthly in the treatment of postmenopausal osteoporosis was assessed in a two year trial which enrolled 1583 patients aged 54 to 81 years, with 395 patients exposed to ibandronate sodium 2.5 mg daily and 396 exposed to ibandronate sodium 150 mg monthly. Patients with active or significant pre-existing gastrointestinal disease were excluded from this trial. Patients with dyspepsia or concomitant use of non-steroidal anti-inflammatory drugs, proton pump inhibitors and H2 antagonists were included in this study. All patients received 500 mg calcium plus 400 international units vitamin D supplementation daily.
After one year, the incidence of all-cause mortality was 0.3% in both the ibandronate sodium 2.5 mg daily group and the ibandronate sodium 150 mg monthly group. The incidence of serious adverse events was 5% in the ibandronate sodium 2.5 mg daily group and 7% in the ibandronate sodium 150 mg monthly group. The percentage of patients who withdrew from treatment due to adverse events was 9% in the ibandronate sodium 2.5 mg daily group and 8% in the ibandronate sodium 150 mg monthly group. Table 2 lists the adverse events reported in greater than or equal to 2% of patients.
| Body System/Adverse Event | Ibandronate Sodium 2.5 mg Daily % (n=395) |
Ibandronate Sodium 150 mg Monthly % (n=396) |
|---|---|---|
| Vascular Disorders | ||
| Hypertension | 7.3 | 6.3 |
| Gastrointestinal Disorders | ||
| Dyspepsia | 7.1 | 5.6 |
| Nausea | 4.8 | 5.1 |
| Diarrhea | 4.1 | 5.1 |
| Constipation | 2.5 | 4.0 |
| Abdominal Paina | 5.3 | 7.8 |
| Musculoskeletal and Connective Tissue Disorders | ||
| Arthralgia | 3.5 | 5.6 |
| Back Pain | 4.3 | 4.5 |
| Pain in Extremity | 1.3 | 4.0 |
| Localized Osteoarthritis | 1.3 | 3.0 |
| Myalgia | 0.8 | 2.0 |
| Muscle Cramp | 2.0 | 1.8 |
| Infections and Infestations | ||
| Influenza | 3.8 | 4.0 |
| Nasopharyngitis | 4.3 | 3.5 |
| Bronchitis | 3.5 | 2.5 |
| Urinary Tract Infection | 1.8 | 2.3 |
| Upper Respiratory Tract Infection | 2.0 | 2.0 |
| Nervous System Disorders | ||
| Headache | 4.1 | 3.3 |
| Dizziness | 1.0 | 2.3 |
| General Disorders and Administration Site Conditions | ||
| Influenza-like Illnessb | 0.8 | 3.3 |
| Skin and Subcutaneous Tissue Disorders | ||
| Rashc | 1.3 | 2.3 |
| Psychiatric Disorders | ||
| Insomnia | 0.8 | 2.0 |
| aCombination of abdominal pain and abdominal pain upper | ||
| bCombination of influenza-like illness and acute phase reaction | ||
| cCombination of rash pruritic, rash macular, rash papular, rash generalized, rash erythematous, dermatitis, dermatitis allergic, dermatitis medicamentosa, erythema and exanthema | ||
Gastrointestinal Adverse Events
The incidence of adverse events in the ibandronate sodium 2.5 mg daily and ibandronate sodium 150 mg monthly groups were: dyspepsia (7% vs. 6%), diarrhea (4% vs. 5%), and abdominal pain (5% vs. 8%).
Musculoskeletal Adverse Events
The incidence of adverse events in the ibandronate sodium 2.5 mg daily and ibandronate sodium 150 mg monthly groups were: back pain (4% vs. 5%), arthralgia (4% vs. 6%) and myalgia (1% vs. 2%).
Acute Phase Reactions
Symptoms consistent with acute phase reactions have been reported with bisphosphonate use. Over the two years of the study, the overall incidence of acute phase reaction symptoms was 3% in the ibandronate sodium 2.5 mg daily group and 9% in the ibandronate sodium 150 mg monthly group. These incidence rates are based on the reporting of any of 33 acute-phase reaction like symptoms within 3 days of the monthly dosing and lasting 7 days or less. Influenza like illness was reported in no patients in the ibandronate sodium 2.5 mg daily group and 2% in the ibandronate sodium 150 mg monthly group.
Ocular Adverse Events
Two patients who received ibandronate sodium 150 mg once-monthly experienced ocular inflammation, one was a case of uveitis and the other scleritis.
One hundred sixty (160) postmenopausal women without osteoporosis participated in a 1-year, double-blind, placebo-controlled study of ibandronate sodium 150 mg once-monthly for prevention of bone loss. Seventy-seven subjects received ibandronate sodium and 83 subjects received placebo. The overall pattern of adverse events was similar to that previously observed.
Postmarketing Experience
The following adverse reactions have been identified during postapproval use of ibandronate sodium. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Hypersensitivity
Allergic reactions including anaphylactic reaction/shock; in some cases fatal, angioedema, bronchospasm, asthma exacerbations, and rash have been reported.
Hypocalcemia
Hypocalcemia has been reported in patients treated with ibandronate sodium.
Musculoskeletal Pain
Bone, joint, or muscle pain (musculoskeletal pain), described as severe or incapacitating, has been reported.
Jaw Osteonecrosis
Osteonecrosis of the jaw has been reported in patients treated with ibandronate sodium.
Atypical Femoral Shaft Fracture
Atypical, low-energy, or low-trauma fractures of the femoral shaft.
DRUG INTERACTIONS
Calcium Supplements/Antacids
Products containing calcium and other multivalent cations (such as aluminum, magnesium, iron) are likely to interfere with absorption of ibandronate sodium. Therefore, instruct patients to take ibandronate sodium at least 60 minutes before any oral medications, including medications containing multivalent cations (such as antacids, supplements or vitamins). Also, patients should wait at least 60 minutes after dosing before taking any other oral medications.
Aspirin/Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
Because aspirin, NSAIDs, and bisphosphonates are all associated with gastrointestinal irritation, caution should be exercised in the concomitant use of aspirin or NSAIDs with ibandronate sodium.
H2 Blockers
In healthy volunteers, coadministration with ranitidine resulted in a 20% increased bioavailability of ibandronate, which was not considered to be clinically relevant.
Drug/Laboratory Test Interactions
Bisphosphonates are known to interfere with the use of bone-imaging agents. Specific studies with ibandronate have not been performed.
USE IN SPECIFIC POPULATIONS
Pregnancy: Category C
There are no adequate and well-controlled studies in pregnant women. Ibandronate sodium should be used during pregnancy only if the potential benefit justifies the potential risk to the mother and fetus.
Bisphosphonates are incorporated into the bone matrix, from where they are gradually released over periods of weeks to years. The extent of bisphosphonate incorporation into adult bone, and hence, the amount available for release back into the systemic circulation, is directly related to the total dose and duration of bisphosphonate use. Although there are no data on fetal risk in humans, bisphosphonates do cause fetal harm in animals, and animal data suggest that uptake of bisphosphonates into fetal bone is greater than into maternal bone. Therefore, there is a theoretical risk of fetal harm (e.g., skeletal and other abnormalities) if a woman becomes pregnant after completing a course of bisphosphonate therapy. The impact of variables such as time between cessation of bisphosphonate therapy to conception, the particular bisphosphonate used, and the route of administration (intravenous versus oral) on this risk has not been established.
In female rats given ibandronate orally at doses greater than or equal to 3 times human exposure at the recommended daily oral dose of 2.5 mg or greater than or equal to 1 times human exposure at the recommended once-monthly oral dose of 150 mg beginning 14 days before mating and continuing through lactation, maternal deaths were observed at the time of delivery in all dose groups. Perinatal pup loss in dams given 45 times human exposure at the recommended daily dose and 13 times the recommended once-monthly dose was likely related to maternal dystocia. Calcium supplementation did not completely prevent dystocia and periparturient mortality in any of the treated groups at greater than or equal to 16 times the recommended daily dose and greater than or equal to 4.6 times the recommended once-monthly dose. A low incidence of postimplantation loss was observed in rats treated from 14 days before mating throughout lactation or during gestation, only at doses causing maternal dystocia and periparturient mortality. In pregnant rats dosed orally from gestation day 17 through lactation day 21 (following closure of the hard palate through weaning), maternal toxicity, including dystocia and mortality, fetal perinatal and postnatal mortality, were observed at doses equivalent to human exposure at the recommended daily and greater than or equal to 4 times the recommended once-monthly dose. Periparturient mortality has also been observed with other bisphosphonates and appears to be a class effect related to inhibition of skeletal calcium mobilization resulting in hypocalcemia and dystocia.
Exposure of pregnant rats during the period of organogenesis resulted in an increased fetal incidence of RPU (renal pelvis ureter) syndrome at oral doses 30 times the human exposure at the recommended daily oral dose of 2.5 mg and greater than or equal to 9 times the recommended once-monthly oral dose of 150 mg. Impaired pup neuromuscular development (cliff avoidance test) was observed at 45 times human exposure at the daily dose and 13 times the once-monthly dose.
In pregnant rabbits treated orally with ibandronate during gestation at doses greater than or equal to 8 times the recommended human daily oral dose of 2.5 mg and greater than or equal to 4 times the recommended human once-monthly oral dose of 150 mg, dose-related maternal mortality was observed in all treatment groups. The deaths occurred prior to parturition and were associated with lung edema and hemorrhage. No significant fetal anomalies were observed.
Nursing Mothers
It is not known whether ibandronate sodium is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when ibandronate sodium is administered to a nursing woman. In lactating rats treated with intravenous doses, ibandronate was present in breast milk from 2 to 24 hours after dose administration. Concentrations in milk averaged 1.5 times plasma concentrations.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
Geriatric Use
Of the patients receiving ibandronate sodium 2.5 mg daily in postmenopausal osteoporosis studies, 52% were over 65 years of age, and 10% were over 75 years of age. Of the patients receiving ibandronate sodium 150 mg once-monthly in the postmenopausal osteoporosis 1-year study, 52% were over 65 years of age, and 9% were over 75 years of age. No overall differences in effectiveness or safety were observed between these patients and younger patients but greater sensitivity in some older individuals cannot be ruled out.
Renal Impairment
Ibandronate sodium is not recommended for use in patients with severe renal impairment (creatinine clearance less than 30 mL/min).
OVERDOSAGE
No specific information is available on the treatment of overdosage of ibandronate sodium. However, based on knowledge of this class of compounds, oral overdosage may result in hypocalcemia, hypophosphatemia, and upper gastrointestinal adverse events, such as upset stomach, dyspepsia, esophagitis, gastritis, or ulcer. Milk or antacids should be given to bind ibandronate sodium. Due to the risk of esophageal irritation, vomiting should not be induced, and the patient should remain fully upright. Dialysis would not be beneficial.
DESCRIPTION
Ibandronate sodium is a nitrogen-containing bisphosphonate that inhibits osteoclast-mediated bone resorption. The chemical name for ibandronate sodium is 3-(N-methyl-N-pentyl) amino-1-hydroxypropane-1,1-diphosphonic acid, monosodium salt, monohydrate with the molecular formula C9H22NO7P2Na•H2O and a molecular weight of 359.24. Ibandronate sodium is a white- to off-white powder. It is freely soluble in water and practically insoluble in organic solvents. Ibandronate sodium has the following structural formula:

Ibandronate sodium is available as a white to off-white, capsule-shaped 150-mg tablet for once-monthly oral administration. One 150-mg tablet contains 168.75 mg ibandronate monosodium monohydrate, equivalent to 150 mg free acid. Ibandronate sodium tablets also contain the following inactive ingredients: sorbitol, microcrystalline cellulose, colloidal anhydrous silica, croscarmellose sodium, sodium stearyl fumarate and Ibandronate sodium II white [polyvinyl alcohol, titanium dioxide, macrogol/PEG 3350 and talc].
CLINICAL PHARMACOLOGY
Mechanism of Action
The action of ibandronate on bone tissue is based on its affinity for hydroxyapatite, which is part of the mineral matrix of bone. Ibandronate inhibits osteoclast activity and reduces bone resorption and turnover. In postmenopausal women, it reduces the elevated rate of bone turnover, leading to, on average, a net gain in bone mass.
Pharmacodynamics
>Osteoporosis is characterized by decreased bone mass and increased fracture risk, most commonly at the spine, hip, and wrist. The diagnosis can be confirmed by a finding of low bone mass, evidence of fracture on x-ray, a history of osteoporotic fracture, or height loss or kyphosis indicative of vertebral fracture. While osteoporosis occurs in both men and women, it is most common among women following menopause. In healthy humans, bone formation and resorption are closely linked; old bone is resorbed and replaced by newly formed bone. In postmenopausal osteoporosis, bone resorption exceeds bone formation, leading to bone loss and increased risk of fracture. After menopause, the risk of fractures of the spine and hip increases; approximately 40% of 50-year-old women will experience an osteoporosis-related fracture during their remaining lifetimes.
Ibandronate sodium produced biochemical changes indicative of dose-dependent inhibition of bone resorption, including decreases of biochemical markers of bone collagen degradation (such as deoxypyridinoline, and cross-linked C-telopeptide of Type I collagen) in the daily dose range of 0.25 mg to 5 mg and once-monthly doses from 100 mg to 150 mg in postmenopausal women.
Treatment with 2.5 mg daily ibandronate sodium resulted in decreases in biochemical markers of bone turnover, including urinary C-terminal telopeptide of Type I collagen (uCTX) and serum osteocalcin, to levels similar to those in premenopausal women. Changes in markers of bone formation were observed later than changes in resorption markers, as expected, due to the coupled nature of bone resorption and formation. Treatment with 2.5 mg daily ibandronate sodium decreased levels of uCTX within 1 month of starting treatment and decreased levels of osteocalcin within 3 months. Bone turnover markers reached a nadir of approximately 64% below baseline values by 6 months of treatment and remained stable with continued treatment for up to 3 years. Following treatment discontinuation, there is a return to pretreatment baseline rates of elevated bone resorption associated with postmenopausal osteoporosis.
In a 1-year, study comparing once-monthly vs. once-daily oral dosing regimens, the median decrease from baseline in serum CTX values was -76% for patients treated with the 150 mg once-monthly regimen and -67% for patients treated with the 2.5 mg daily regimen. In a 1-year, prevention study comparing ibandronate sodium 150 mg once-monthly to placebo, the median placebo-subtracted decrease in sCTX was -49.8%.
Pharmacokinetics
Absorption
The absorption of oral ibandronate occurs in the upper gastrointestinal tract. Plasma concentrations increase in a dose-linear manner up to 50 mg oral intake and increases nonlinearly above this dose.
Following oral dosing, the time to maximum observed plasma ibandronate concentrations ranged from 0.5 to 2 hours (median 1 hour) in fasted healthy postmenopausal women. The mean oral bioavailability of 2.5 mg ibandronate was about 0.6% compared to intravenous dosing. The extent of absorption is impaired by food or beverages (other than plain water). The oral bioavailability of ibandronate is reduced by about 90% when ibandronate sodium is administered concomitantly with a standard breakfast in comparison with bioavailability observed in fasted subjects. There is no meaningful reduction in bioavailability when ibandronate is taken at least 60 minutes before a meal. However, both bioavailability and the effect on bone mineral density (BMD) are reduced when food or beverages are taken less than 60 minutes following an ibandronate dose.
Distribution
After absorption, ibandronate either rapidly binds to bone or is excreted into urine. In humans, the apparent terminal volume of distribution is at least 90 L, and the amount of dose removed from the circulation via the bone is estimated to be 40% to 50% of the circulating dose. In vitro protein binding in human serum was 99.5% to 90.9% over an ibandronate concentration range of 2 to 10 ng/mL in one study and approximately 85.7% over a concentration range of 0.5 to 10 ng/mL in another study.
Metabolism
Ibandronate does not undergo hepatic metabolism and does not inhibit the hepatic cytochrome P450 system. Ibandronate is eliminated by renal excretion. Based on a rat study, the ibandronate secretory pathway does not appear to include known acidic or basic transport systems involved in the excretion of other drugs. There is no evidence that ibandronate is metabolized in humans.
Elimination
The portion of ibandronate that is not removed from the circulation via bone absorption is eliminated unchanged by the kidney (approximately 50% to 60% of the absorbed dose). Unabsorbed ibandronate is eliminated unchanged in the feces.
The plasma elimination of ibandronate is multiphasic. Its renal clearance and distribution into bone accounts for a rapid and early decline in plasma concentrations, reaching 10% of the Cmax within 3 or 8 hours after intravenous or oral administration, respectively. This is followed by a slower clearance phase as ibandronate redistributes back into the blood from bone. The observed apparent terminal half-life for ibandronate is generally dependent on the dose studied and on assay sensitivity. The observed apparent terminal half-life for the 150 mg ibandronate tablet upon oral administration to healthy postmenopausal women ranges from 37 to 157 hours.
Total clearance of ibandronate is low, with average values in the range 84 to 160 mL/min. Renal clearance (about 60 mL/min in healthy postmenopausal females) accounts for 50% to 60% of total clearance and is related to creatinine clearance. The difference between the apparent total and renal clearances likely reflects bone uptake of the drug.
Specific Populations
Pediatrics
The pharmacokinetics of ibandronate has not been studied in patients less than 18 years of age.
Geriatric
Because ibandronate is not known to be metabolized, the only difference in ibandronate elimination for geriatric patients versus younger patients is expected to relate to progressive age-related changes in renal function.
Gender
The bioavailability and pharmacokinetics of ibandronate are similar in both men and women.
Race
Pharmacokinetic differences due to race have not been studied.
Renal Impairment
Renal clearance of ibandronate in patients with various degrees of renal impairment is linearly related to creatinine clearance (CLcr).
Following a single dose of 0.5 mg ibandronate by intravenous administration, patients with CLcr 40 to 70 mL/min had 55% higher exposure (AUC∞) than the exposure observed in subjects with CLcr greater than 90 mL/min. Patients with CLcr less than 30 mL/min had more than a two-fold increase in exposure compared to the exposure for healthy subjects (see Dosage and Administration).
Hepatic Impairment
No studies have been performed to assess the pharmacokinetics of ibandronate in patients with hepatic impairment because ibandronate is not metabolized in the human liver.
Drug Interaction Studies
Products containing calcium and other multivalent cations (such as aluminum, magnesium, iron), including milk, food, and antacids are likely to interfere with absorption of ibandronate, which is consistent with findings in animal studies.
H2 Blockers
A pharmacokinetic interaction study in healthy volunteers demonstrated that 75 mg ranitidine (25 mg injected intravenously 90 and 15 minutes before and 30 minutes after ibandronate administration) increased the oral bioavailability of 10 mg ibandronate by about 20%. This degree of increase is not considered to be clinically relevant.
NONCLINICAL TOXICOLOGY
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
In a 104-week carcinogenicity study, doses of 3, 7, or 15 mg/kg/day were administered by oral gavage to male and female Wistar rats (systemic exposures up to 12 and 7 times, respectively, human exposure at the recommended daily oral dose of 2.5 mg, and cumulative exposures up to 3.5 and 2 times, respectively, human exposure at the recommended once-monthly oral dose of 150 mg, based on AUC comparison). There were no significant drug-related tumor findings in male or female rats. In a 78-week carcinogenicity study, doses of 5, 20, or 40 mg/kg/day were administered by oral gavage to male and female NMRI mice (exposures up to 475 and 70 times, respectively, human exposure at the recommended daily oral dose of 2.5 mg and cumulative exposures up to 135 and 20 times, respectively, human exposure at the recommended once-monthly oral dose of 150 mg, based on AUC comparison). There were no significant drug-related tumor findings in male or female mice. In a 90-week carcinogenicity study, doses of 5, 20, or 80 mg/kg/day were administered in the drinking water to NMRI mice (cumulative monthly exposures in males and females up to 70 and 115 times, respectively, human exposure at the recommended dose of 150 mg, based on AUC comparison). A dose-related increased incidence of adrenal subcapsular adenoma/carcinoma was observed in female mice, which was statistically significant at 80 mg/kg/day (220 to 400 times human exposure at the recommended daily oral dose of 2.5 mg and 115 times human exposure at the recommended once-monthly oral dose of 150 mg, based on AUC comparison). The relevance of these findings to humans is unknown.
Mutagenesis
There was no evidence for a mutagenic or clastogenic potential of ibandronate in the following assays: in vitro bacterial mutagenesis assay in Salmonella typhimurium and Escherichia coli (Ames test), mammalian cell mutagenesis assay in Chinese hamster V79 cells, and chromosomal aberration test in human peripheral lymphocytes, each with and without metabolic activation. Ibandronate was not genotoxic in the in vivo mouse micronucleus tests for chromosomal damage.
Impairment of Fertility
In female rats treated from 14 days prior to mating through gestation, decreases in fertility, corpora lutea, and implantation sites were observed at an oral dose of 16 mg/kg/day (45 times human exposure at the recommended daily oral dose of 2.5 mg and 13 times human exposure at the recommended once-monthly oral dose of 150 mg, based on AUC comparison).
Animal Reproductive and Developmental Toxicology
In female rats given oral doses of 1, 4, or 16 mg/kg/day beginning 14 days before mating and continuing through lactation, maternal deaths were observed at the time of delivery in all dose groups (greater than or equal to 3 times human exposure at the recommended daily oral dose of 2.5 mg or greater than or equal to 1 times human exposure at the recommended once-monthly oral dose of 150 mg, based on AUC comparison). Perinatal pup loss in dams given 16 mg/kg/day (45 times human exposure at the recommended daily oral dose of 2.5 mg and 13 times human exposure at the recommended once-monthly oral dose of 150 mg, based on AUC comparison) was likely related to maternal dystocia. In pregnant rats given oral doses of 6, 20, or 60 mg/kg/day during gestation, calcium supplementation (32 mg/kg/day by subcutaneous injection from gestation day 18 to parturition) did not completely prevent dystocia and periparturient mortality in any of the treated groups (greater than or equal to 16 times human exposure at the recommended daily oral dose of 2.5 mg and greater than or equal to 4.6 times human exposure at the recommended once-monthly oral dose of 150 mg, based on AUC comparison). A low incidence of postimplantation loss was observed in rats treated from 14 days before mating throughout lactation or during gestation, only at doses causing maternal dystocia and periparturient mortality. In pregnant rats dosed orally with 1, 5, or 20 mg/kg/day from gestation day 17 through lactation day 21 (following closure of the hard palate through weaning), maternal toxicity, including dystocia and mortality, fetal perinatal and postnatal mortality, were observed at doses greater than or equal to 5 mg/kg/day (equivalent to human exposure at the recommended daily oral dose of 2.5 mg and greater than or equal to 4 times human exposure at the recommended once-monthly oral dose of 150 mg, based on AUC comparison). Periparturient mortality has also been observed with other bisphosphonates and appears to be a class effect related to inhibition of skeletal calcium mobilization resulting in hypocalcemia and dystocia.
Exposure of pregnant rats during the period of organogenesis resulted in an increased fetal incidence of RPU (renal pelvis ureter) syndrome at oral doses greater than or equal to 10 mg/kg/day (greater than or equal to 30 times human exposure at the recommended daily oral dose of 2.5 mg and greater than or equal to 9 times human exposure at the recommended once-monthly oral dose of 150 mg, based on AUC comparison). Impaired pup neuromuscular development (cliff avoidance test) was observed at 16 mg/kg/day when dams were dosed from 14 days before mating through lactation (45 times human exposure at the recommended daily oral dose of 2.5 mg and 13 times human exposure at the recommended once-monthly oral dose of 150 mg, based on AUC comparison).
In pregnant rabbits given oral doses of 1, 4, or 20 mg/kg/day during gestation, dose-related maternal mortality was observed in all treatment groups (greater than or equal to 8 times the recommended human daily oral dose of 2.5 mg and greater than or equal to 4 times the recommended human once-monthly oral dose of 150 mg, based on body surface area comparison, mg/m2). The deaths occurred prior to parturition and were associated with lung edema and hemorrhage. No significant fetal anomalies were observed.
Animal Pharmacology
Animal studies have shown that ibandronate is an inhibitor of osteoclast-mediated bone resorption. In the Schenk assay in growing rats, ibandronate inhibited bone resorption and increased bone volume, based on histologic examination of the tibial metaphyses. There was no evidence of impaired mineralization at the highest dose of 5 mg/kg/day (subcutaneously), which is 1000 times the lowest antiresorptive dose of 0.005 mg/kg/day in this model, and 5000 times the optimal antiresorptive dose of 0.001 mg/kg/day in the aged ovariectomized rat. This indicates that ibandronate sodium administered at therapeutic doses is unlikely to induce osteomalacia.
Long-term daily or once-monthly intermittent administration of ibandronate to ovariectomized rats or monkeys was associated with suppression of bone turnover and increases in bone mass. In both rats and monkeys, vertebral BMD, trabecular density, and biomechanical strength were increased dose-dependently at doses up to 15 times the recommended human daily oral dose of 2.5 mg, or cumulative monthly doses up to 8 times (rat) or 6 times (monkey) the recommended human once-monthly oral dose of 150 mg, based on body surface area (mg/m2) or AUC comparison. In monkeys, ibandronate maintained the positive correlation between bone mass and strength at the ulna and femoral neck. New bone formed in the presence of ibandronate had normal histologic structure and did not show mineralization defects.
CLINICAL STUDIES
Treatment of Postmenopausal Osteoporosis
Daily Dosing
The effectiveness and safety of ibandronate sodium were demonstrated in a randomized, double-blind, placebo-controlled, multinational study (Treatment Study) of 2946 women aged 55 to 80 years, who were on average 21 years postmenopause, who had lumbar spine BMD 2 to 5 SD below the premenopausal mean (T-score) in at least one vertebra [L1-L4], and who had 1 to 4 prevalent vertebral fractures. ibandronate sodium was evaluated at oral doses of 2.5 mg daily and 20 mg intermittently. The main outcome measure was the occurrence of new radiographically diagnosed vertebral fractures after 3 years of treatment. The diagnosis of an incident vertebral fracture was based on both qualitative diagnosis by the radiologist and quantitative morphometric criterion. The morphometric criterion required the dual occurrence of 2 events: a relative height ratio or relative height reduction in a vertebral body of at least 20%, together with at least a 4 mm absolute decrease in height. All women received 400 international units vitamin D and 500 mg calcium supplementation per day.
Effect on Fracture Incidence
Ibandronate sodium 2.5 mg daily significantly reduced the incidence of new vertebral (primary efficacy measure) and of new and worsening vertebral fractures. Over the course of the 3-year study, the risk for vertebral fracture was 9.6% in the placebo-treated women and 4.7% in the women treated with ibandronate sodium 2.5 mg (p<0.001) (see Table 3).
| Proportion of Patients with Fracture (%) | ||||
|---|---|---|---|---|
| Placebo | Ibandronate Sodium 2.5 mg Daily |
Absolute Risk Reduction (%) |
Relative Risk Reduction (%) |
|
| n=975 | n=977 | 95% CI | 95% CI | |
| New Vertebral Fracture | 9.6 | 4.7 | 4.9 | 52** |
| 0-3 Year | (2.3, 7.4) | (29, 68) | ||
| New and Worsening Vertebral Fracture | 10.4 | 5.1 | 5.3 | 52 |
| 0-3 Year | (2.6, 7.9) | (30, 67) | ||
| Clinical (Symptomatic) Vertebral Fracture | 5.3 | 2.8 | 2.5 | 49 |
| 0-3 Year | (0.6, 4.5) | (14, 69) | ||
| *The endpoint value is the value at the study's last time point, 3 years, for all patients who had a fracture identified at that time; otherwise, the last postbaseline value prior to the study's last time point is used. | ||||
| **p=0.0003 vs. placebo | ||||
Ibandronate sodium 2.5 mg daily did not reduce the incidence of nonvertebral fractures (secondary efficacy measure). There was a similar number of nonvertebral osteoporotic fractures at 3 years reported in women treated with ibandronate sodium 2.5 mg daily [9.1%, (95% CI: 7.1%, 11.1%)] and placebo [8.2%, (95% CI: 6.3%, 10.2%)]. The two treatment groups were also similar with regard to the number of fractures reported at the individual nonvertebral sites: pelvis, femur, wrist, forearm, rib, and hip.
Bone Mineral Density (BMD)
Ibandronate sodium significantly increased BMD at the lumbar spine and hip relative to treatment with placebo. In the 3-year osteoporosis treatment study, ibandronate sodium 2.5 mg daily produced increases in lumbar spine BMD that were progressive over 3 years of treatment and were statistically significant relative to placebo at 6 months and at all later time points. Lumbar spine BMD increased by 6.4% after 3 years of treatment with 2.5 mg daily ibandronate sodium compared with 1.4% in the placebo group. Table 4 displays the significant increases in BMD seen at the lumbar spine, total hip, femoral neck, and trochanter compared to placebo.
| Placebo | Ibandronate Sodium 2.5 mg Daily | |
|---|---|---|
| Lumbar Spine | 1.4 | 6.4 |
| (n=693) | (n=712) | |
| Total Hip | -0.7 | 3.1 |
| (n=638) | (n=654) | |
| Femoral Neck | -0.7 | 2.6 |
| (n=683) | (n=699) | |
| Trochanter | 0.2 | 5.3 |
| (n=683) | (n=699) | |
| *The endpoint value is the value at the study's last time point, 3 years, for all patients who had BMD measured at that time; otherwise, the last postbaseline value prior to the study's last time point is used. | ||
Bone Histology
The effects of ibandronate sodium 2.5 mg daily on bone histology were evaluated in iliac crest biopsies from 16 women after 22 months of treatment and 20 women after 34 months of treatment.
The histological analysis of bone biopsies showed bone of normal quality and no indication of osteomalacia or a mineralization defect.
Once-Monthly Dosing
The effectiveness and safety of ibandronate sodium once-monthly were demonstrated in a randomized, double-blind, multinational, noninferiority trial in 1602 women aged 54 to 81 years, who were on average 18 years postmenopause, and had L2-L4 lumbar spine BMD T-score below -2.5 SD at baseline. The main outcome measure was the comparison of the percentage change from baseline in lumbar spine BMD after 1 year of treatment with once-monthly ibandronate (100 mg, 150 mg) to daily ibandronate (2.5 mg). All patients received 400 international units vitamin D and 500 mg calcium supplementation per day.
Ibandronate sodium 150 mg once-monthly (n=327) was shown to be noninferior to ibandronate sodium 2.5 mg daily (n=318) in lumbar spine BMD in a 1-year, double-blind, multicenter study of women with postmenopausal osteoporosis. In the primary efficacy analysis (per-protocol population), the mean increases from baseline in lumbar spine BMD at 1 year were 3.86% (95% CI: 3.40%, 4.32%) in the 2.5 mg daily group and 4.85% (95% CI: 4.41%, 5.29%) in the 150 mg once-monthly group; the mean difference between 2.5 mg daily and 150 mg once-monthly was 0.99% (95% CI: 0.38%, 1.60%), which was statistically significant (p=0.002). The results of the intent-to-treat analysis were consistent with the primary efficacy analysis. The 150 mg once-monthly group also had consistently higher BMD increases at the other skeletal sites compared to the 2.5 mg daily group.
Prevention of Postmenopausal Osteoporosis
Daily Dosing
The safety and effectiveness of ibandronate sodium 2.5 mg daily for the prevention of postmenopausal osteoporosis were demonstrated in a randomized, double-blind, placebo-controlled 2-year study (Prevention Study) of 653 postmenopausal women without osteoporosis at baseline. Women were aged 41 to 82 years, were on average 8.5 years postmenopause, and had lumbar spine BMD T-scores greater than -2.5. Women were stratified according to time since menopause (1 to 3 years, greater than 3 years) and baseline lumbar spine BMD (T-score: greater than -1, -1 to -2.5). The study compared daily ibandronate sodium at three dose levels (0.5 mg, 1.0 mg, 2.5 mg) with placebo. All women received 500 mg of supplemental calcium per day.
The primary efficacy measure was the change in BMD of lumbar spine after 2 years of treatment. Ibandronate sodium 2.5 mg daily resulted in a mean increase in lumbar spine BMD of 3.1% compared with placebo following 2 years of treatment. Increases in BMD were seen at 6 months and at all later time points. Irrespective of the time since menopause or the degree of pre-existing bone loss, treatment with ibandronate sodium resulted in a higher BMD response at the lumbar spine compared with placebo across all four baseline strata [time since menopause (1 to 3 years, greater than 3 years) and baseline lumbar spine BMD (T-score: greater than -1, -1 to -2.5)].
Compared with placebo, treatment with ibandronate sodium 2.5 mg daily increased BMD of the total hip by 1.8%, the femoral neck by 2.0%, and the trochanter by 2.1%.
Once-Monthly Dosing
The safety and effectiveness of ibandronate sodium 150 mg once-monthly for the prevention of postmenopausal osteoporosis were demonstrated in a randomized, double-blind, placebo-controlled 1-year study (Monthly Prevention Study) of 160 postmenopausal women with low bone mass at baseline (T-score of -1 to -2.5). Women, aged 46 to 60 years, were on average 5.4 years postmenopause. All women received 400 international units of vitamin D and 500 mg calcium supplementation daily.
The primary efficacy measure was the relative change in BMD at the lumbar spine after 1 year of treatment. Ibandronate sodium 150 mg once-monthly resulted in a mean increase in lumbar spine BMD of 4.12% (95% confidence interval 2.96 – 5.28) compared with placebo following 1 year of treatment (p<0.0001), based on a 3.73% and -0.39% mean change in BMD from baseline in the 150 mg once-monthly ibandronate sodium and placebo treatment groups, respectively. BMD at other skeletal sites was also increased relative to baseline values.
HOW SUPPLIED/STORAGE AND HANDLING
How Supplied
Ibandronate sodium tablets, 150 mg (ibandronate): supplied as white to off-white, capsule-shaped tablets with “IN 150” on one side and ∃ on the other side and packaged in:
Carton of 3 blister packs, each blister containing 1 tablet
Storage and Handling
Store at 20°C - 25°C (68°F - 77°F) [See USP Controlled Room Temperature].
PATIENT COUNSELING INFORMATION
“See FDA-approved patient labeling Medication Guide)”
Information for Patients
Instruct patients to read the Medication Guide carefully before taking ibandronate sodium tablets and to re-read it each time the prescription is renewed because it contains important information the patient should know about ibandronate sodium tablets. The Medication Guide also includes the dosing instructions in order to maximize absorption and clinical benefit.
- Ibandronate sodium tablets should be taken at least 60 minutes before the first food or drink (other than water) of the day and before taking any oral medication or supplementation including calcium, antacids or vitamins (see Drug Interactions).
- To facilitate delivery to the stomach, and thus reduce the potential for esophageal irritation, ibandronate sodium tablets should be swallowed whole with a full glass of plain water (6 to 8 oz) while the patient is standing or sitting in an upright position. Patients should not lie down for 60 minutes after taking ibandronate sodium tablets.
- Patients should not eat, drink anything except for water, or take other medications for 60 minutes after taking ibandronate sodium tablets.
- Plain water is the only drink that should be taken with ibandronate sodium tablets. Note that some mineral waters may have a higher concentration of calcium and therefore should not be used.
- Patients should not chew or suck the tablet because of a potential for oropharyngeal ulceration.
- The ibandronate sodium 150 mg tablet should be taken on the same date each month (i.e., the patient’s ibandronate sodium tablet day).
- The patient must not take two 150 mg tablets within the same week.
- If the once-monthly dose is missed, and the patient’s next scheduled ibandronate sodium tablet day is more than 7 days away, the patient should be instructed to take one ibandronate sodium 150 mg tablet in the morning following the date that it is remembered (see Dosage and Administration [2.3]. The patient should then return to taking one ibandronate sodium 150 mg tablet every month in the morning of their chosen day, according to their original schedule.
- If the once-monthly dose is missed, and the patient’s next scheduled ibandronate sodium tablet day is only 1 to 7 days away, the patient must wait until the subsequent month’s scheduled ibandronate sodium tablet day to take their tablet. The patient should then return to taking one ibandronate sodium 150 mg tablet every month in the morning of their chosen day, according to their original schedule.
Patients should receive supplemental calcium and vitamin D if dietary intake is inadequate. Intake of supplemental calcium and vitamin D should be delayed for at least 60 minutes following oral administration of ibandronate sodium tablets in order to maximize absorption of ibandronate sodium.
Physicians should be alert to signs or symptoms signaling a possible esophageal reaction during therapy, and patients should be instructed to discontinue ibandronate sodium tablets and seek medical attention if they develop symptoms of esophageal irritation such as new or worsening dysphagia, pain on swallowing, retrosternal pain, or heartburn.
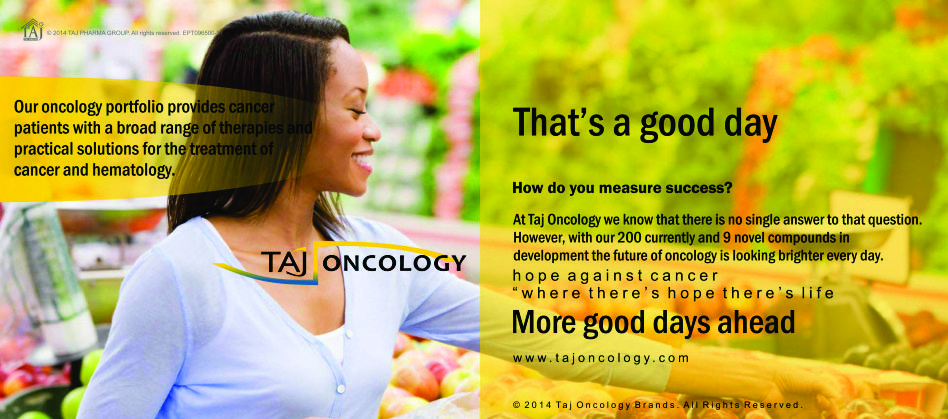
Product Glimpse
Description
We are committed to work towards a healthier and happier world. The company is an integrated, research based international pharmaceutical company, producing a wide range of quality, affordable generic (Ibandronate sodium 50mg Tablets) medicines, trusted by health-care professionals and patients across geographies.
We offer you the highest quality new Generic medicines ie. Ibandronate sodium 50mg Tablets, drugs and also with innovative packing at the lowest prices shipped to you from India. Browse our latest Pharmaceuticals and Generics possibilities and other pharmaceuticals possibilities…more.