Fludarabine 50mg Injection
Fludarabine
Fludarabine 50mg Injection
Fludarabine Phosphate for Injection, USP is supplied as a white, lyophilized solid cake. Each vial contains 50 mg of fludarabine phosphate, USP, 50 mg of mannitol, and sodium hydroxide to adjust pH to 7.7. The pH range for the final product is 7.2 to 8.2. Store at 20 to 25°C (68 to 77°F). [See USP Controlled Room Temperature.] Store upright.
Fludarabine Phosphate for Injection, USP is supplied in a clear glass single dose vial and cartoned individually.
Fludarabine Phosphate for Injection, USP contains fludarabine phosphate, USP, a fluorinated nucleotide analog of the antiviral agent vidarabine, 9-β-D-arabinofuranosyladenine (ara-A) that is relatively resistant to deamination by adenosine deaminase. Each vial of sterile lyophilized solid cake contains 50 mg of the active ingredient fludarabine phosphate, USP, 50 mg of mannitol, and sodium hydroxide to adjust pH to 7.7. The pH range for the final product is 7.2 to 8.2. Reconstitution with 2 mL of Sterile Water for Injection, USP results in a solution containing 25 mg/mL of fludarabine phosphate, USP intended for intravenous administration.
Fludarabine Phosphate for Injection, USP is indicated for the treatment of adult patients with B-cell chronic lymphocytic leukemia (CLL) who have not responded to or whose disease has progressed during treatment with at least one standard alkylating-agent containing regimen. The safety and effectiveness of fludarabine phosphate, USP in previously untreated or non-refractory patients with CLL have not been established.
Fludarabine
Fludarabine 50mg Injection
What Fludarabine Phosphate is and what it is used for
Fludarabine Phosphate is an anti-cancer drug.
Fludarabine Phosphate is used to treat chronic B-cell lymphocytic leukaemia (B-CLL) in patients with sufficient healthy blood cell production. This is a type of cancer of white blood cells (the cells are called lymphocytes).
First treatment for chronic lymphocytic leukaemia with Fludarabine Phosphate should only be started in patients with advanced disease having disease related symptoms or evidence of disease progression.
What you need to know before you use Fludarabine Phosphate
Do not use Fludarabine Phosphate
- if you are allergic to fludarabine phosphate or any of the other ingredients of this medicine (listed in section 6)
- if you are breast-feeding
- if your kidney function is severely impaired
- if you have a low number of red blood cells, because of a certain type of anaemia (decompensated haemolytic anaemia). Your doctor will have told you if you have this condition.
Warnings and precautions
- If you are not feeling very well you should tell your doctor, as your doctor may decide not to give you this medicine, or may give you this medicine with caution. This is very important if your bone marrow is not working properly or if you are susceptible to infections.
- If you notice any unusual bruising, excessive bleeding after injury or if you seem to be catching a lot of infections, tell your doctor. The number of normal blood cells may be reduced and so you will have regular blood tests during treatment.
- The disease itself and the therapy may cause a reduction of the number of blood cells and your immune system may attack different parts of your body (autoimmune disorder). It may also be directed against your red blood cells (called ‘autoimmune haemolysis’). This condition can be life threatening. If this condition occurs you may receive further medication such as transfusion of blood (irradiated, see below) and corticosteroids.
- If you need a blood transfusion and you are being (or have been) treated with this medicine, you should mention this to the doctor. Your doctor will ensure that you receive blood only, which has gone through a special treatment (irradiation). There have been severe complications and even death reported when non-irradiated blood has been given.
- If you need to have stem cells collected and you are being (or have been) treated with this medicine, you should mention this to the doctor.
- If your liver does not work properly, your doctor may give you this medicine with caution.
- If you have any form of kidney disease, your kidney function should be checked regularly. If it is found that your kidneys do not work properly you may be given this medicine at a reduced dose.
If your kidneys work at only a very low level you will not be given this medicine at all. Patients aged 65 years or older should have their kidney function checked before start of treatment. - There is little information on the effects of Fludarabine Phosphate in patients aged 75 years and older. Your doctor will use it with caution if you are in this age group.
- If you have very severe chronic lymphocytic leukaemia, your body may not be able to get rid of all the waste products from the cells destroyed by Fludarabine Phosphate. This is called tumour lysis syndrome and may cause dehydration, kidney failure and heart problems. Your doctor will be aware of this and may give you other medicines to stop this happening.
- If you experience any unusual symptoms from the nervous system you should mention it to your doctor. This is because when used in patients at doses four times greater than the recommended dose, severe central nervous system (brain and spinal cord) effects including blindness, coma and death have been reported.
- Tell your doctor if you notice any changes to your skin either while you are receiving this medicine or after you have finished the course of therapy. The doctor should check the seriousness of the skin changes. If you have skin cancer, the damaged areas of your skin may become worse when you use this medicine.
- Men and women who may still be fertile, must use a reliable form of contraception during and for at least 6 months after stopping treatment.
- Check with your doctor about any vaccinations you may need, because live vaccinations should be avoided during and after treatment with Fludarabine Phosphate.
Children and adolescents
Fludarabine Phosphate is not recommended for use in children and adolescents below age 18.
No data are available concerning the use of Fludarabine Phosphate in the paediatric population.
Other medicines and Fludarabine Phosphate
Tell your doctor if you are taking, have recently taken or might take any other medicines. This is especially important if you are taking a drug called pentostatin or deoxycoformycin (also used to treat chronic lymphocytic leukaemia) as a combination with Fludarabine Phosphate is not recommended. Some drugs, e.g. dipyridamole (used to prevent excessive blood clotting) may reduce the effectiveness of Fludarabine Phosphate.
It is especially important to tell your doctor about:
- pentostatin (deoxycoformycin), also used to treat B-CLL. Taking these two drugs together can lead to severe lung problems.
- dipyridamole, used to prevent excessive blood clotting or other similar substances. They may reduce the effectiveness of Fludarabine Phosphate.
- cytarabine (Ara-C) used to treat chronic lymphatic leukaemia. If Fludarabine Phosphate is combined with cytarabine, levels of the active form of Fludarabine Phosphate in leukaemic cells may rise. However, the overall levels in the blood and its elimination from the blood were not shown to have changed.
Pregnancy, breast-feeding and fertility
If you are pregnant or breast-feeding, think you may be pregnant or are planning to have a baby, ask your doctor or pharmacist for advice before taking this medicine.
Fludarabine Phosphate treatment has the potential to harm the unborn child. You should not be given Fludarabine Phosphate if you are pregnant unless clearly necessary and when the potential benefits justify the potential risks to the unborn child. If you are a woman who may still be fertile, you must avoid becoming pregnant during treatment and for at least 6 months after stopping treatment. However, if you do become pregnant inform your doctor immediately.
Men who are treated with Fludarabine Phosphate and can father a child must use a reliable form of contraception during, and for at least 6 months after stopping treatment.
It is not known if this medicine appears in the breast milk of women treated with Fludarabine Phosphate. However, in animal studies the medicinal product was found in breast milk. Therefore you must not breast feed during your treatment with this medicine.
Driving and using machines
Some people get tired, feel weak, have disturbed vision, become confused or agitated or have seizures while they are treated with Fludarabine Phosphate. Do not try to drive or operate machines until you are sure that you are not affected.
Fludarabine Phosphate contains sodium
This medicinal contains less than 1mmol sodium (23mg) per ml, i.e. essentially ‘sodium-free’.
How to use Fludarabine Phosphate
Fludarabine Phosphate should be administered under the supervision of a qualified doctor experienced in cancer therapy.
The dose you are given depends on the size of your body. It varies with your body surface area. Technically this is measured in square metres (m2), but actually is worked out from your height and weight. The recommended dose is 25 mg/m2 body surface. This will be given either as an injection or as an infusion (with a drip) into a vein once a day for 5 consecutive days every 28 days. This five day course of treatment will be repeated every 28 days until your doctor has decided that the best effect has been achieved (usually after 6 cycles). The dosage may be decreased or the repeat course delayed if side effects are a problem. If you have kidney problems or if you are over the age of 65, you will have regular tests to check your kidney function. If your kidneys do not work properly you may be given this medicine at a lower dose. If your kidney function is severely reduced you will not be given this medicine at all (see also section 2, ‘Do not use Fludarabine Phosphate’).
The safety of this drug in children and adolescents below age 18 has not been established and treatment is not recommended.
If any of the Fludarabine Phosphate solution comes into contact with your skin or the lining of your nose or mouth, wash the area thoroughly with soap and water. If the solution gets into your eyes, rinse them thoroughly with lots of water. Try not to breathe in any fumes coming from the solution.
If you use more Fludarabine Phosphate than you should
In the case of an overdose your doctor will stop the therapy and treat the symptoms.
Symptoms of an overdose can be blindness which may not appear until later, coma and death due to irreversible toxicity to the central nervous system. High doses can also lead to a severely reduced number of blood cells.
If you forget to use Fludarabine Phosphate
Your doctor will set the times at which you are to receive this medicine. If you think you may have missed a dose, contact your doctor as soon as possible.
If you have any further questions on the use of this product, ask your doctor or pharmacist.
Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
If you are not sure what the adverse reactions below are, ask your doctor to explain them to you.
Some side effects can be life-threatening.
- If you have difficulty breathing, have a cough or have chest pain with or without fever. These may be signs of an infection of the lungs.
- If you notice any unusual bruising, more bleeding than usual after injury or if you seem to be catching a lot of infections. These may be caused by a reduced number of blood cells. This may also lead to an increased risk of (serious) infections, caused by organisms, that usually do not cause disease in healthy persons (opportunistic infections) including a late reactivation of viruses, for example herpes zoster.
- If you notice any pain in your side, blood in your urine or reduced amount of urine. These may be signs of tumour lysis syndrome (see 2 ‘Warnings and precautions’).
- If you notice any skin and / or mucous coat reaction with redness, inflammation, blistering and tissue break down. These may be signs of a severe allergic reaction (Lyell’s syndrome, Stevens-Johnson syndrome).
- If you have palpitations (if you suddenly become aware of your heart beat) or chest pain. These may be signs of heart problems.
Tell your doctor immediately, if you notice any of these effects.
Below we list possible side effects by how common they are. The rare side effects (less than 1 in every 1000 patients) were mainly identified from post-marketing experience.
Very common means 1 or more in every 10 patients are likely to get these:
- infections (some serious)
- infections due to depressed immune system (opportunistic infections)
- infection of the lungs (pneumonia) with possible symptoms like breathing difficulties and/or cough with or without fever
- reduction in the number of blood platelets (thrombocytopenia) with the possibility of bruising and bleeding
- lowered white blood cell count (neutropenia)
- lowered red blood cell count (anaemia)
- cough
- vomiting, diarrhoea, feeling sick (nausea)
- fever
- feeling tired (fatigue)
- weakness.
Common means between 1 and 10 in every 100 patients are likely to get these:
- other blood related cancers (myelodysplastic syndrome, acute myeloid leukaemia). Most patients with these conditions were previously, or at the same time or later treated with other cancer drugs (alkylating agents, topoisomerase inhibitors) or radiation therapy
- bone marrow depression (myelosuppression)
- severe loss of appetite leading to weight loss (anorexia)
- numbness or weakness in limbs (peripheral neuropathy)
- disturbed vision
- inflammation of the inside of the mouth (stomatitis)
- skin rash
- swelling due to excessive fluid retention (oedema)
- inflammation of the mucous coat of the digestive system from the mouth to the anus (mucositis)
- chills
- generally feeling unwell.
Uncommon means between 1 and 10 in every 1,000 patients are likely to get these:
- attack of the immune system on parts of the body or red blood cells (autoimmune disorder)
- increase in potassium, phosphate and uric acid in the blood that can cause kidney problems (tumour lysis syndrome)
- confusion
- lung toxicity; scaring throughout the lungs (pulmonary fibrosis), inflammation of the lungs (pneumonitis), shortness of breath (dyspnoea)
- bleeding in the stomach or intestines
- abnormal levels of the liver or pancreas enzymes.
Rare means less than 10 in every 10,000 patients are likely to get these:
- disorders of the lymph system due to a viral infection (EBV-associated lymphoproliferative disorder)
- coma
- seizures
- agitation
- blindness
- inflammation or damage of the nerve of the eyes (optic neuritis; optic neuropathy)
- heart failure
- irregular heart beat (arrhythmia)
- skin cancer
- skin and/or mucous coat reaction with redness, inflammation, blistering and tissue break down (Lyell’s syndrome, Stevens-Johnson syndrome).
Frequency not know
- inflammation of the bladder, which can cause pain when passing urine, and can lead to blood in the urine (haemorrhagic cystitis)
- bleeding in the brain (cerebral haemorrhage)
- bleeding in the lungs (pulmonary haemorrhage).
If you get any side effects, talk to your doctor. This includes any side effects not listed in this leaflet.
How to store Fludarabine Phosphate
Keep this medicine out of the sight and reach of children.
Store the vial before opening between 2-8°C.
The diluted solution of Fludarabine Phosphate in 0.9% sodium chloride is stable for up to 28 days in PVC and PE bags at 2-8°C and at 25°C when protected from light.
From a microbiological point of view, the product must be used immediately. If not used immediately, in-use storage times and conditions prior to use are the responsibility of the user and would normally not be longer than 24 hours at 2 to 8°C, unless dilution has taken place in controlled and validated aseptic conditions.
Do not use this medicine after the expiry date which is stated on the carton and vial after EXP.
Do not throw away any medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. These measures will help protect the environment.
Contents of the pack and other information
What Fludarabine Phosphate contains
- The active substance is fludarabine phosphate 1 ml concentrate contains 25 mg fludarabine phosphate.
Each 2 ml vial contains 50 mg fludarabine phosphate. - The other ingredients are disodium phosphate dihydrate, water for injections, sodium hydroxide (for pH adjustment).
What Fludarabine Phosphate looks like and contents of the pack
Fludarabine Phosphate is a clear, colourless or almost colourless solution.
Colourless glass vial (type I) with bromobutylic rubber stopper and metallic cap (aluminium) with polypropylene disk. Vial will be packed with or without a protective plastic overwrap.
Pack sizes
- 1 x 2 ml vial
- 5 x 2 ml vial
Not all pack sizes may be marketed.
Fludarabine
Fludarabine 50mg Injection
DESCRIPTION
Fludarabine Phosphate for Injection, USP contains fludarabine phosphate, USP, a fluorinated nucleotide analog of the antiviral agent vidarabine, 9-β-D-arabinofuranosyladenine (ara-A) that is relatively resistant to deamination by adenosine deaminase. Each vial of sterile lyophilized solid cake contains 50 mg of the active ingredient fludarabine phosphate, USP, 50 mg of mannitol, and sodium hydroxide to adjust pH to 7.7. The pH range for the final product is 7.2 to 8.2. Reconstitution with 2 mL of Sterile Water for Injection, USP results in a solution containing 25 mg/mL of fludarabine phosphate, USP intended for intravenous administration.
The chemical name for fludarabine phosphate, USP is 9H-Purin-6-amine, 2-fluoro-9-(5-O-phosphono- β - D-arabinofuranosyl)(2-fluoro-ara-AMP). The molecular formula of fludarabine phosphate, USP is C10H13FN5O7P (MW 365.2) and the structure is:

CLINICAL PHARMACOLOGY
Fludarabine phosphate, USP is rapidly dephosphorylated to 2-fluoro-ara-A and then phosphorylated intracellularly by deoxycytidine kinase to the active triphosphate, 2-fluoro-ara-ATP. This metabolite appears to act by inhibiting DNA polymerase alpha, ribonucleotide reductase and DNA primase, thus inhibiting DNA synthesis. The mechanism of action of this antimetabolite is not completely characterized and may be multi-faceted.
Phase I studies in humans have demonstrated that fludarabine phosphate, USP is rapidly converted to the active metabolite, 2-fluoro-ara-A, within minutes after intravenous infusion. Consequently, clinical pharmacology studies have focused on 2-fluoro-ara-A pharmacokinetics. After the five daily doses of 25 mg 2-fluoro-ara-AMP/m2 to cancer patients infused over 30 minutes, 2-fluoro-ara-A concentrations show a moderate accumulation. During a 5-day treatment schedule, 2-fluoro-ara-A plasma trough levels increased by a factor of about 2. The terminal half-life of 2-fluoro-ara-A was estimated as approximately 20 hours. In vitro, plasma protein binding of fludarabine ranged between 19% and 29%.
A correlation was noted between the degree of absolute granulocyte count nadir and increased area under the concentration x time curve (AUC).
Special Populations
Pediatric Patients
Limited pharmacokinetic data for fludarabine phosphate, USP are available from a published study of children (ages 1 to 21 years) with refractory acute leukemias or solid tumors (Children’s Cancer Group Study 0971). When fludarabine phosphate, USP was administered as a loading dose over 10 minutes immediately followed by a 5-day continuous infusion, steady-state conditions were reached early.
Patients with Renal Impairment
The total body clearance of the principal metabolite 2-fluoro-ara-A correlated with the creatinine clearance, indicating the importance of the renal excretion pathway for the elimination of the drug. Renal clearance represents approximately 40% of the total body clearance. Patients with moderate renal impairment (17 to 41 mL/min/m2) receiving 20% reduced fludarabine phosphate, USP dose had a similar exposure (AUC; 21 versus 20 nM•h/mL) compared to patients with normal renal function receiving the recommended dose. The mean total body clearance was 172 mL/min for normal and 124 mL/min for patients with moderately impaired renal function.
Clinical Studies
Two single-arm open-label studies of fludarabine phosphate, USP have been conducted in adult patients with CLL refractory to at least one prior standard alkylating-agent containing regimen. In a study conducted by M.D. Anderson Cancer Center (MDAH), 48 patients were treated with a dose of 22 to 40 mg/m2 daily for 5 days every 28 days. Another study conducted by the Southwest Oncology Group (SWOG) involved 31 patients treated with a dose of 15 to 25 mg/m2 daily for 5 days every 28 days. The overall objective response rates were 48% and 32% in the MDAH and SWOG studies, respectively. The complete response rate in both studies was 13%; the partial response rate was 35% in the MDAH study and 19% in the SWOG study. These response rates were obtained using standardized response criteria developed by the National Cancer Institute CLL Working Group3 and were achieved in heavily pre-treated patients. The ability of fludarabine phosphate, USP to induce a significant rate of response in refractory patients suggests minimal cross-resistance with commonly used anti-CLL agents.
The median time to response in the MDAH and SWOG studies was 7 weeks (range of 1 to 68 weeks) and 21 weeks (range of 1 to 53 weeks) respectively. The median duration of disease control was 91 weeks (MDAH) and 65 weeks (SWOG). The median survival of all refractory CLL patients treated with fludarabine phosphate, USP was 43 weeks and 52 weeks in the MDAH and SWOG studies, respectively.
Rai stage improved to Stage II or better in 7 of 12 MDAH responders (58%) and in 5 of 7 SWOG responders (71%) who were Stage III or IV at baseline. In the combined studies, mean hemoglobin concentration improved from 9.0 g/dL at baseline to 11.8 g/dL at the time of response in a subgroup of anemic patients. Similarly, average platelet count improved from 63,500/mm3 to 103,300/mm3 at the time of response in a subgroup of patients who were thrombocytopenic at baseline.
INDICATIONS AND USAGE
Fludarabine Phosphate for Injection, USP is indicated for the treatment of adult patients with B-cell chronic lymphocytic leukemia (CLL) who have not responded to or whose disease has progressed during treatment with at least one standard alkylating-agent containing regimen. The safety and effectiveness of fludarabine phosphate, USP in previously untreated or non-refractory patients with CLL have not been established.
CONTRAINDICATIONS
Fludarabine phosphate, USP is contraindicated in those patients who are hypersensitive to this drug or its components.
WARNINGS
(See BOXED WARNINGS)
There are clear dose-dependent toxic effects seen with fludarabine phosphate, USP. Dose levels approximately 4 times greater (96 mg/m2/day for 5 to 7 days) than that recommended for CLL (25 mg/m2/day for 5 days) were associated with a syndrome characterized by delayed blindness, coma and death. Symptoms appeared from 21 to 60 days following the last dose. Thirteen of 36 patients (36%) who received fludarabine phosphate, USP at high doses (96 mg/m2/day for 5 to 7 days) developed this severe neurotoxicity. Similar severe central nervous system toxicity, including coma, seizures, agitation and confusion, has been reported in patients treated at doses in the range of the dose recommended for chronic lymphocytic leukemia.
The effect of chronic administration of fludarabine phosphate, USP on the central nervous system is unknown; however, patients have received the recommended dose for up to 15 courses of therapy.
Severe bone marrow suppression, notably anemia, thrombocytopenia and neutropenia, has been reported in patients treated with fludarabine phosphate, USP. In a Phase I study in adult solid tumor patients, the median time to nadir counts was 13 days (range, 3 to 25 days) for granulocytes and 16 days (range, 2 to 32) for platelets. Most patients had hematologic impairment at baseline either as a result of disease or as a result of prior myelosuppressive therapy. Cumulative myelosuppression may be seen. While chemotherapy-induced myelosuppression is often reversible, administration of fludarabine phosphate, USP requires careful hematologic monitoring.
Several instances of trilineage bone marrow hypoplasia or aplasia resulting in pancytopenia, sometimes resulting in death, have been reported in adult patients. The duration of clinically significant cytopenia in the reported cases has ranged from approximately 2 months to approximately 1 year. These episodes have occurred both in previously treated or untreated patients.
Instances of life-threatening and sometimes fatal autoimmune phenomena such as hemolytic anemia, autoimmune thrombocytopenia / thrombocytopenic purpura (ITP), Evan’s syndrome, and acquired hemophilia have been reported to occur after one or more cycles of treatment with fludarabine phosphate, USP in patients with or without a previous history of autoimmune hemolytic anemia or a positive Coombs’ test and who may or may not be in remission from their disease. Steroids may or may not be effective in controlling these hemolytic episodes. The majority of patients rechallenged with fludarabine phosphate, USP developed a recurrence in the hemolytic process. The mechanism(s) which predispose patients to the development of this complication has not been identified. Patients undergoing treatment with fludarabine phosphate, USP should be evaluated and closely monitored for hemolysis. Discontinuation of therapy with fludarabine phosphate, USP is recommended in case of hemolysis.
Transfusion-associated graft-versus-host disease has been observed after transfusion of non-irradiated blood in fludarabine phosphate, USP treated patients. Fatal outcome as a consequence of this disease has been reported. Therefore, to minimize the risk of transfusion-associated graft-versus-host disease, patients who require blood transfusion and who are undergoing, or who have received, treatment with fludarabine phosphate, USP should receive irradiated blood only.
In a clinical investigation using fludarabine phosphate, USP in combination with pentostatin (deoxycoformycin) for the treatment of refractory chronic lymphocytic leukemia (CLL) in adults, there was an unacceptably high incidence of fatal pulmonary toxicity. Therefore, the use of fludarabine phosphate, USP in combination with pentostatin is not recommended.
Of the 133 adult CLL patients in the two trials, there were 29 fatalities during study. Approximately 50% of the fatalities were due to infection and 25% due to progressive disease.
Pregnancy Category D:
Based on its mechanism of action, fludarabine phosphate, USP can cause fetal harm when administered to a pregnant woman. There are no adequate and well-controlled studies of fludarabine phosphate, USP in pregnant women. Fludarabine phosphate was embryolethal and teratogenic in both rats and rabbits. If fludarabine phosphate, USP is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus. Women of childbearing potential should be advised to avoid becoming pregnant. Women of childbearing potential and fertile males must take contraceptive measures during and at least for six months after cessation of treatment with fludarabine phosphate, USP.
Fludarabine phosphate, USP was embryolethal and teratogenic in rats and rabbits.
Fludarabine phosphate, USP was administered at doses of 0, 1, 10 or 30 mg/kg/day (0.24, 2.4 times and 7.2 times the recommended human dose on a mg/m2 basis, respectively) to pregnant rats on days 6 to 15 of gestation. At 10 and 30 mg/kg/day administered during organogenesis, there was a dose-related increase in various skeletal variations and a decrease in mean fetal body weights. Maternal toxicity was not apparent at 10 mg/kg/day, and was limited to slight body weight decreases at 30 mg/kg/day. In a dose finding study malformations, such as limb and tail defects, were induced at 40 mg/kg/day (9.6 times the recommended human dose on a mg/m2 basis). In a reproduction toxicity study on rabbits Fludarabine phosphate was administered intravenously at doses of 0, 1, 5 or 8 mg/kg/day (approximately 0.5, 2.4, and 3.8 times the recommended human dose on a mg/m2 basis) on days 6 to 18 of gestation. A dose of 8 mg/kg/day administered during organogenesis increased embryo and fetal lethality as indicated by a higher number of resorptions and a decrease in live fetuses. Compound-related teratogenic effects manifested by external deformities and skeletal malformations were observed at 8 mg/kg/day. The most frequent external malformations observed in rabbits were cleft palate, adactyly, brachydactyly and syndactyly along with skeletal malformations such as fused metatarsals, phalanges, sternebrae and limb bones and some soft tissue malformations (diaphragmatic herniae). Fetal body weights were decreased in rabbits given 8 mg/kg/day.
PRECAUTIONS
General
Fludarabine phosphate, USP is a potent antineoplastic agent with potentially significant toxic side effects. Patients undergoing therapy should be closely observed for signs of hematologic and nonhematologic toxicity. Periodic assessment of peripheral blood counts is recommended to detect the development of anemia, neutropenia and thrombocytopenia.
Tumor lysis syndrome associated with fludarabine phosphate, USP treatment has been reported in CLL patients with large tumor burdens. Since fludarabine phosphate, USP can induce a response as early as the first week of treatment, precautions should be taken in those patients at risk of developing this complication.
In patients with impaired state of health, fludarabine phosphate, USP should be given with caution and after careful risk/benefit consideration. This applies especially for patients with severe impairment of bone marrow function (thrombocytopenia, anemia, and/or granulocytopenia), immunodeficiency or with a history of opportunistic infection. Prophylactic treatment should be considered in patients at increased risk of developing opportunistic infections.
There are inadequate data on dosing of patients with renal insufficiency. Fludarabine phosphate, USP must be administered cautiously in patients with renal insufficiency. The total body clearance of 2-fluoro-ara-A has been shown to be directly correlated with creatinine clearance. Patients with moderate impairment of renal function (creatinine clearance 30 to 70 mL/min/1.73 m2) should have their fludarabine dose reduced by 20% and be monitored closely. Fludarabine is not recommended for patients with severely impaired renal function (creatinine clearance less than 30 mL/min/1.73 m2).
Fludarabine phosphate, USP may reduce the ability to drive or use machines, since fatigue, weakness, visual disturbances, confusion, agitation and seizures have been observed.
Laboratory Tests
During treatment, the patient’s hematologic profile (particularly neutrophils and platelets) should be monitored regularly to determine the degree of hematopoietic suppression.
Drug Interactions
The use of fludarabine phosphate, USP in combination with pentostatin is not recommended due to the risk of severe pulmonary toxicity (see WARNINGS section).
Carcinogenesis
No animal carcinogenicity studies with fludarabine phosphate, USP have been conducted.
Mutagenesis
Fludarabine phosphate, USP was not mutagenic to bacteria (Ames test) or mammalian cells (HGRPT assay in Chinese hamster ovary cells) either in the presence or absence of metabolic activation. Fludarabine phosphate, USP was clastogenic in vitro to Chinese hamster ovary cells (chromosome aberrations in the presence of metabolic activation) and induced sister chromatid exchanges both with and without metabolic activation. In addition, fludarabine phosphate, USP was clastogenic in vivo (mouse micronucleus assay) but was not mutagenic to germ cells (dominant lethal test in male mice).
Impairment of Fertility
Studies in mice, rats and dogs have demonstrated dose-related adverse effects on the male reproductive system. Observations consisted of a decrease in mean testicular weights in mice and rats with a trend toward decreased testicular weights in dogs and degeneration and necrosis of spermatogenic epithelium of the testes in mice, rats and dogs. The possible adverse effects on fertility in humans have not been adequately evaluated.
Pregnancy
Pregnancy Category D:
(See WARNINGS section).
Nursing Mothers
It is not known whether fludarabine phosphate, USP is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions including tumorgenicity in nursing infants, a decision should be made to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
Data submitted to the FDA was insufficient to establish efficacy in any childhood malignancy. Fludarabine was evaluated in 62 pediatric patients (median age 10, range 1 to 21) with refractory acute leukemia (45 patients) or solid tumors (17 patients). The fludarabine regimen tested for pediatric acute lymphocytic leukemia (ALL) patients was a loading bolus of 10.5 mg/m2/day followed by a continuous infusion of 30.5 mg/m2/day for 5 days. In 12 pediatric patients with solid tumors, dose-limiting myelosuppression was observed with a loading dose of 8 mg/m2/day followed by a continuous infusion of 23.5 mg/m2/day for 5 days. The maximum tolerated dose was a loading dose of 7 mg/m2/day followed by a continuous infusion of 20 mg/m2/day for 5 days. Treatment toxicity included bone marrow suppression. Platelet counts appeared to be more sensitive to the effects of fludarabine than hemoglobin and white blood cell counts. Other adverse events included fever, chills, asthenia, rash, nausea, vomiting, diarrhea, and infection. There were no reported occurrences of peripheral neuropathy or pulmonary hypersensitivity reaction.
Vaccination
During and after treatment with fludarabine phosphate, USP, vaccination with live vaccines should be avoided.
Disease Progression
Disease progression and transformation (e.g. Richter’s syndrome) have been reported in CLL patients.
ADVERSE REACTIONS
The most common adverse events include myelosuppression (neutropenia, thrombocytopenia and anemia), fever and chills, infection, and nausea and vomiting. Other commonly reported events include malaise, fatigue, anorexia, and weakness. Serious opportunistic infections have occurred in CLL patients treated with fludarabine phosphate, USP. Adverse events, and those reactions which are more clearly related to the drug are arranged below according to body system.
Hematopoietic Systems:
Hematologic events (neutropenia, thrombocytopenia, and/or anemia) were reported in the majority of CLL patients treated with fludarabine phosphate, USP. During fludarabine phosphate, USP treatment of 133 patients with CLL, the absolute neutrophil count decreased to less than 500/mm3 in 59% of patients, hemoglobin decreased from pretreatment values by at least 2 grams percent in 60%, and platelet count decreased from pretreatment values by at least 50% in 55%. Myelosuppression may be severe, cumulative, and may affect multiple cell lines. Bone marrow fibrosis occurred in one CLL patient treated with fludarabine phosphate, USP.
Several instances of trilineage bone marrow hypoplasia or aplasia resulting in pancytopenia, sometimes resulting in death, have been reported in postmarketing surveillance. The duration of clinically significant cytopenia in the reported cases has ranged from approximately 2 months to approximately 1 year. These episodes have occurred both in previously treated or untreated patients.
Life-threatening and sometimes fatal autoimmune phenomena such as hemolytic anemia, autoimmune thrombocytopenia/thrombocytopenic purpura (ITP), Evan’s syndrome, and acquired hemophilia have been reported to occur in patients receiving fludarabine phosphate, USP. The majority of patients rechallenged with fludarabine phosphate, USP developed a recurrence in the hemolytic process.
In post-marketing experience, cases of myelodysplastic syndrome and acute myeloid leukemia mainly associated with prior, concomitant or subsequent treatment with alkylating agents, topoisomerase inhibitors, or irradiation have been reported.
Infections:
Serious, and sometimes fatal infections, including opportunistic infections and reactivations of latent viral infections such as VZV (Herpes zoster), Epstein-Barr virus and JC virus (progressive multifocal leukoencephalopathy) have been reported in patients treated with fludarabine phosphate, USP.
Rare cases of Epstein Barr Virus (EBV) associated lymphoproliferative disorders have been reported in patients treated with fludarabine phosphate, USP.
Metabolic:
Tumor lysis syndrome has been reported in CLL patients treated with fludarabine phosphate, USP. This complication may include hyperuricemia, hyperphosphatemia, hypocalcemia, metabolic acidosis, hyperkalemia, hematuria, urate crystalluria, and renal failure. The onset of this syndrome may be heralded by flank pain and hematuria.
Nervous System:
Objective weakness, agitation, confusion, seizures, visual disturbances, optic neuritis, optic neuropathy, blindness and coma have occurred in CLL patients treated with fludarabine phosphate, USP at the recommended dose. Peripheral neuropathy has been observed in patients treated with fludarabine phosphate, USP and one case of wrist-drop was reported.
In post-marketing experience, cases of progressive multifocal leukoencephalopathy have been reported. Most cases had a fatal outcome. Many of these cases were confounded by prior and/or concurrent chemotherapy. The time to onset has ranged from a few weeks to approximately one year after initiating treatment.
Pulmonary System:
Pneumonia, a frequent manifestation of infection in CLL patients, occurred in 16%, and 22% of those treated with fludarabine phosphate, USP in the MDAH and SWOG studies, respectively. Pulmonary hypersensitivity reactions to fludarabine phosphate, USP characterized by dyspnea, cough and interstitial pulmonary infiltrate have been observed.
In post-marketing experience, cases of severe pulmonary toxicity have been observed with fludarabine use which resulted in ARDS, respiratory distress, pulmonary hemorrhage, pulmonary fibrosis, and respiratory failure. After an infectious origin has been excluded, some patients experienced symptom improvement with corticosteroids.
Gastrointestinal System:
Gastrointestinal disturbances such as nausea and vomiting, anorexia, diarrhea, stomatitis, and gastrointestinal bleeding have been reported in patients treated with fludarabine phosphate, USP.
Cardiovascular:
Edema has been frequently reported. One patient developed a pericardial effusion possibly related to treatment with fludarabine phosphate, USP. No other severe cardiovascular events were considered to be drug related.
Genitourinary System:
Rare cases of hemorrhagic cystitis have been reported in patients treated with fludarabine phosphate, USP.
Skin:
Skin toxicity, consisting primarily of skin rashes, has been reported in patients treated with fludarabine phosphate, USP.
Erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis, and pemphigus have been reported, with fatal outcomes in some cases.
Worsening or flare up of pre-existing skin cancer lesions, as well as new onset of skin cancer, has been reported in patients during or after treatment with fludarabine phosphate, USP.
Data in the following table are derived from the 133 patients with CLL who received fludarabine phosphate, USP in the MDAH and SWOG studies.
| ADVERSE EVENTS | MDAH (N=101) | SWOG (N=32) |
|---|---|---|
| ANY ADVERSE EVENT | 88% | 91% |
| BODY AS A WHOLE | 72 | 84 |
| FEVER | 60 | 69 |
| CHILLS | 11 | 19 |
| FATIGUE | 10 | 38 |
| INFECTION | 33 | 44 |
| PAIN | 20 | 22 |
| MALAISE | 8 | 6 |
| DIAPHORESIS | 1 | 13 |
| ALOPECIA | 0 | 3 |
| ANAPHYLAXIS | 1 | 0 |
| HEMORRHAGE | 1 | 0 |
| HYPERGLYCEMIA | 1 | 6 |
| DEHYDRATION | 1 | 0 |
| NEUROLOGICAL | 21 | 69 |
| WEAKNESS | 9 | 65 |
| PARESTHESIA | 4 | 12 |
| HEADACHE | 3 | 0 |
| VISUAL DISTURBANCE | 3 | 15 |
| HEARING LOSS | 2 | 6 |
| SLEEP DISORDER | 1 | 3 |
| DEPRESSION | 1 | 0 |
| CEREBELLAR SYNDROME | 1 | 0 |
| IMPAIRED MENTATION | 1 | 0 |
| PULMONARY | 35 | 69 |
| COUGH | 10 | 44 |
| PNEUMONIA | 16 | 22 |
| DYSPNEA | 9 | 22 |
| SINUSITIS | 5 | 0 |
| PHARYNGITIS | 0 | 9 |
| UPPER RESPIRATORY INFECTION | 2 | 16 |
| ALLERGIC PNEUMONITIS | 0 | 6 |
| EPISTAXIS | 1 | 0 |
| HEMOPTYSIS | 1 | 6 |
| BRONCHITIS | 1 | 0 |
| HYPOXIA | 1 | 0 |
| GASTROINTESTINAL | 46 | 63 |
| NAUSEA/VOMITING | 36 | 31 |
| DIARRHEA | 15 | 13 |
| ANOREXIA | 7 | 34 |
| STOMATITIS | 9 | 0 |
| GI BLEEDING | 3 | 13 |
| ESOPHAGITIS | 3 | 0 |
| MUCOSITIS | 2 | 0 |
| LIVER FAILURE | 1 | 0 |
| ABNORMAL LIVER FUNCTION TEST | 1 | 3 |
| CHOLELITHIASIS | 0 | 3 |
| CONSTIPATION | 1 | 3 |
| DYSPHAGIA | 1 | 0 |
| CUTANEOUS | 17 | 18 |
| RASH | 15 | 15 |
| PRURITUS | 1 | 3 |
| SEBORRHEA | 1 | 0 |
| GENITOURINARY | 12 | 22 |
| DYSURIA | 4 | 3 |
| URINARY INFECTION | 2 | 15 |
| HEMATURIA | 2 | 3 |
| RENAL FAILURE | 1 | 0 |
| ABNORMAL RENAL FUNCTION TEST | 1 | 0 |
| PROTEINURIA | 1 | 0 |
| HESITANCY | 0 | 3 |
| CARDIOVASCULAR | 12 | 38 |
| EDEMA | 8 | 19 |
| ANGINA | 0 | 6 |
| CONGESTIVE HEART FAILURE | 0 | 3 |
| ARRHYTHMIA | 0 | 3 |
| SUPRAVENTRICULAR TACHYCARDIA | 0 | 3 |
| MYOCARDIAL INFARCTION | 0 | 3 |
| DEEP VENOUS THROMBOSIS | 1 | 3 |
| PHLEBITIS | 1 | 3 |
| TRANSIENT ISCHEMIC ATTACK | 1 | 0 |
| ANEURYSM | 1 | 0 |
| CEREBROVASCULAR ACCIDENT /td> | 0 | 3 |
| MUSCULOSKELETAL | 7 | 16 |
| MYALGIA | 4 | 16 |
| OSTEOPOROSIS | 2 | 0 |
| ARTHRALGIA | 1 | 0 |
| TUMOR LYSIS SYNDROME | 1 | 0 |
More than 3000 adult patients received fludarabine phosphate, USP in studies of other leukemias, lymphomas, and other solid tumors. The spectrum of adverse effects reported in these studies was consistent with the data presented above.
OVERDOSAGE
High doses of fludarabine phosphate, USP have been associated with an irreversible central nervous system toxicity characterized by delayed blindness, coma, and death. High doses are also associated with severe thrombocytopenia and neutropenia due to bone marrow suppression. There is no known specific antidote for fludarabine phosphate, USP overdosage. Treatment consists of drug discontinuation and supportive therapy.
DOSAGE AND ADMINISTRATION
Usual Dose:
The recommended adult dose of Fludarabine Phosphate for Injection, USP is 25 mg/m2 administered intravenously over a period of approximately 30 minutes daily for five consecutive days. Each 5 day course of treatment should commence every 28 days. Dosage may be decreased or delayed based on evidence of hematologic or nonhematologic toxicity. Physicians should consider delaying or discontinuing the drug if neurotoxicity occurs.
A number of clinical settings may predispose to increased toxicity from fludarabine phosphate, USP. These include advanced age, renal insufficiency, and bone marrow impairment. Such patients should be monitored closely for excessive toxicity and the dose modified accordingly.
The optimal duration of treatment has not been clearly established. It is recommended that three additional cycles of fludarabine phosphate, USP be administered following the achievement of a maximal response and then the drug should be discontinued.
Renal Insufficiency
Adult patients with moderate impairment of renal function (creatinine clearance 30 to 70 mL/min/1.73 m2) should have a 20% dose reduction of fludarabine phosphate, USP. Fludarabine phosphate, USP should not be administered to patients with severely impaired renal function (creatinine clearance less than 30 mL/min/1.73 m2).
Preparation of Solutions:
Fludarabine Phosphate for Injection, USP should be prepared for parenteral use by aseptically adding Sterile Water for Injection, USP. When reconstituted with 2 mL of Sterile Water for Injection, USP, the solid cake should fully dissolve in 15 seconds or less; each mL of the resulting solution will contain 25 mg of fludarabine phosphate, USP, 25 mg of mannitol, and sodium hydroxide to adjust the pH to 7.7. The pH range for the final product is 7.2 to 8.2. In clinical studies, the product has been diluted in 100 cc or 125 cc of 5% Dextrose Injection, USP or 0.9% Sodium Chloride, USP.
Reconstituted Fludarabine Phosphate for Injection, USP contains no antimicrobial preservative and thus should be used within 8 hours of reconstitution. Care must be taken to assure the sterility of prepared solutions. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration.
Fludarabine Phosphate for Injection, USP should not be mixed with other drugs.
Handling and Disposal:
Procedures for proper handling and disposal should be considered. Consideration should be given to handling and disposal according to guidelines issued for cytotoxic drugs. Several guidelines on this subject have been published.1-4
Caution should be exercised in the handling and preparation of Fludarabine Phosphate for Injection, USP solution. The use of latex gloves and safety glasses is recommended to avoid exposure in case of breakage of the vial or other accidental spillage. If the solution contacts the skin or mucous membranes, wash thoroughly with soap and water; rinse eyes thoroughly with plain water. Avoid exposure by inhalation or by direct contact of the skin or mucous membranes.
HOW SUPPLIED
Fludarabine Phosphate for Injection, USP is supplied as a white, lyophilized solid cake. Each vial contains 50 mg of fludarabine phosphate, USP, 50 mg of mannitol, and sodium hydroxide to adjust pH to 7.7. The pH range for the final product is 7.2 to 8.2. Store at 20 to 25°C (68 to 77°F). [See USP Controlled Room Temperature.] Store upright.
Fludarabine Phosphate for Injection, USP is supplied in a clear glass single dose vial and cartoned individually.
REFERENCES
- Preventing Occupational Exposures to Antineoplastic and Other Hazardous Drugs in Health Care Settings. NIOSH Alert 2004-165.
- OSHA Technical Manual, TED 1-0.15A, Section VI: Chapter 2. Controlling Occupational Exposure to Hazardous Drugs. OSHA, 1999. http://www.osha.gov/dts/osta/otm/otm_vi_2.html
- American Society of Health-System Pharmacists. ASHP guidelines on handling hazardous drugs. Am J Health-Syst Pharm. 2006: 63: 1172-1193.
- Polvich, M., White, J.M., & Kelleher, L.O. (eds.) 2005. Chemotherapy and biotherapy guidelines and recommendations for practice (2nd ed.).Pittsburgh,PA: Oncology Nursing Society.
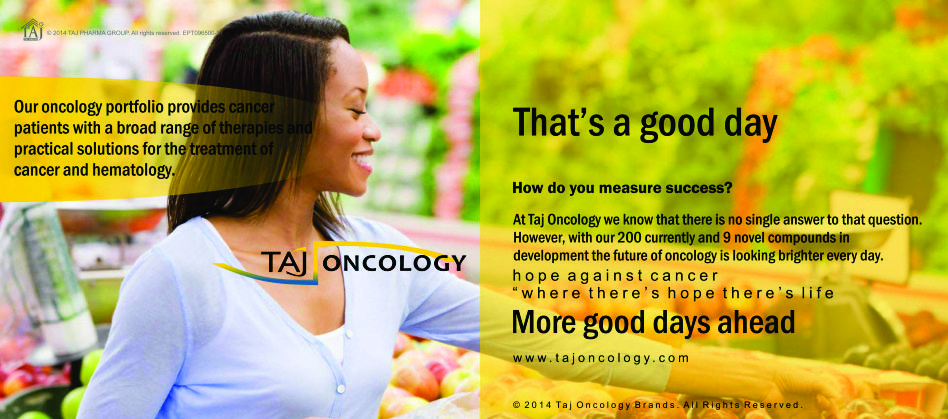
Product Glimpse
Description
We are committed to work towards a healthier and happier world. The company is an integrated, research based international pharmaceutical company, producing a wide range of quality, affordable generic (Fludarabine 50mg Injection) medicines, trusted by health-care professionals and patients across geographies.
We offer you the highest quality new Generic medicines ie. Fludarabine 50mg Injection, drugs and also with innovative packing at the lowest prices shipped to you from India. Browse our latest Pharmaceuticals and Generics possibilities and other pharmaceuticals possibilities…more.