Etoposide 100mg/5ml Injection
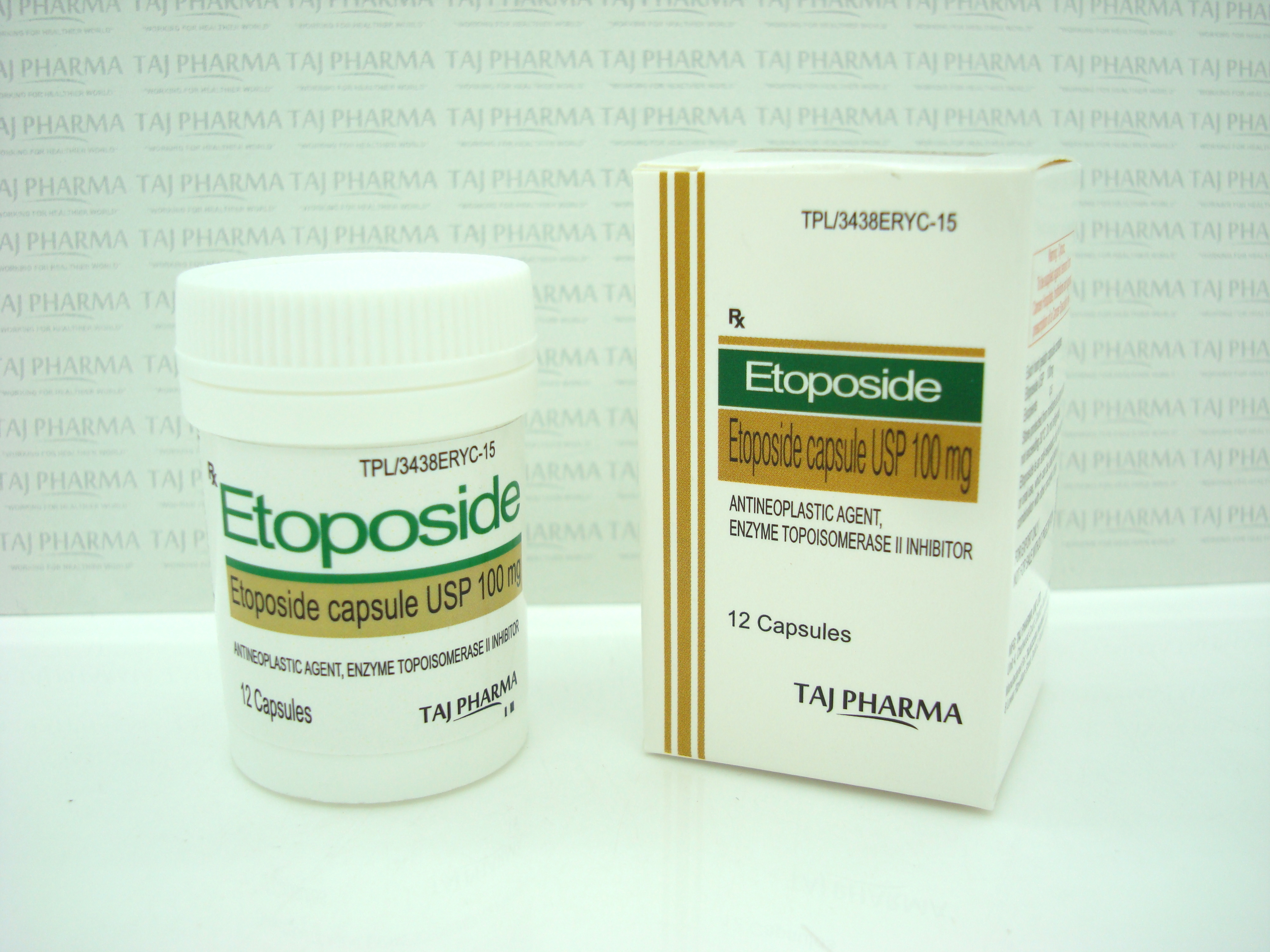
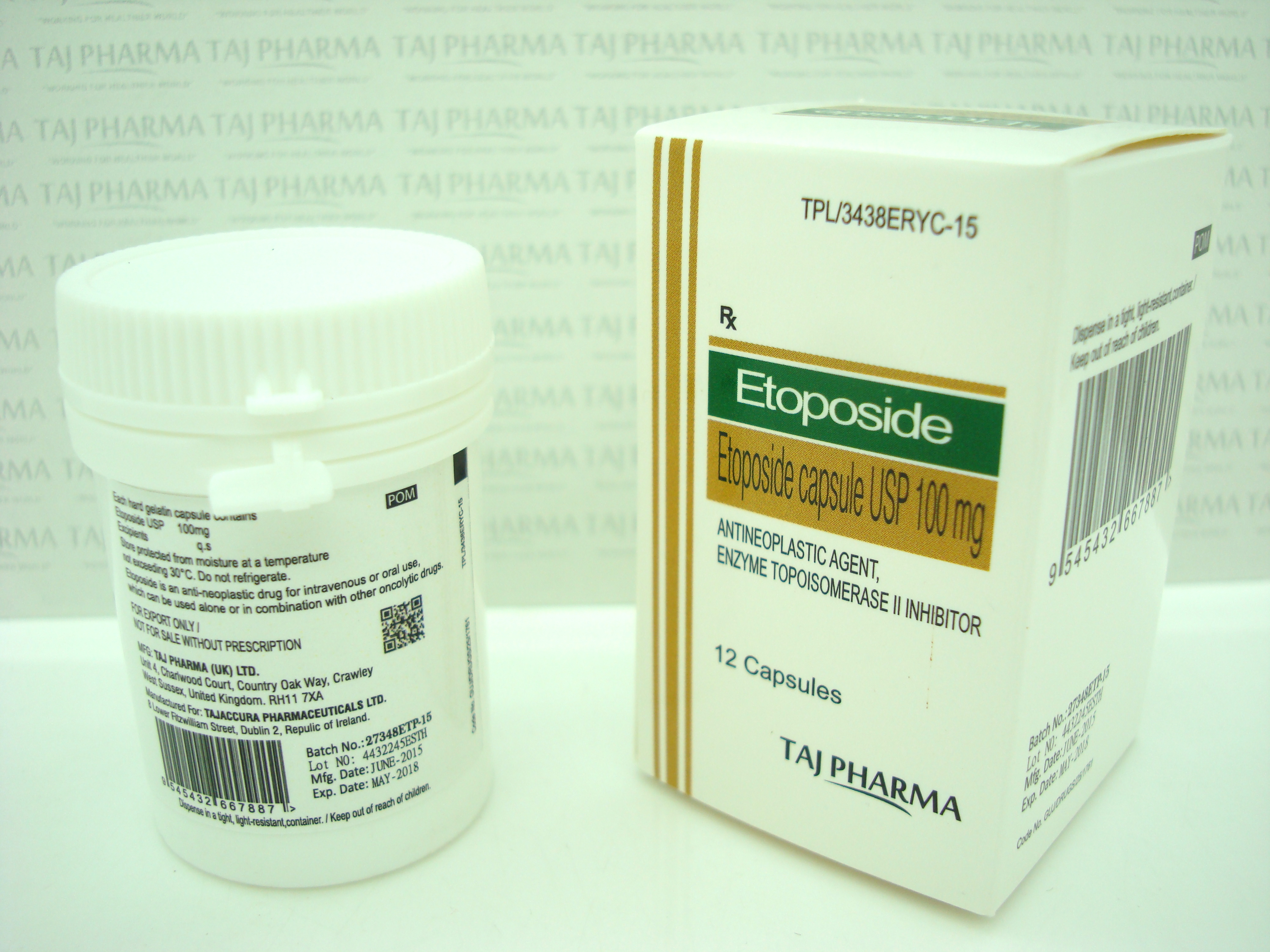
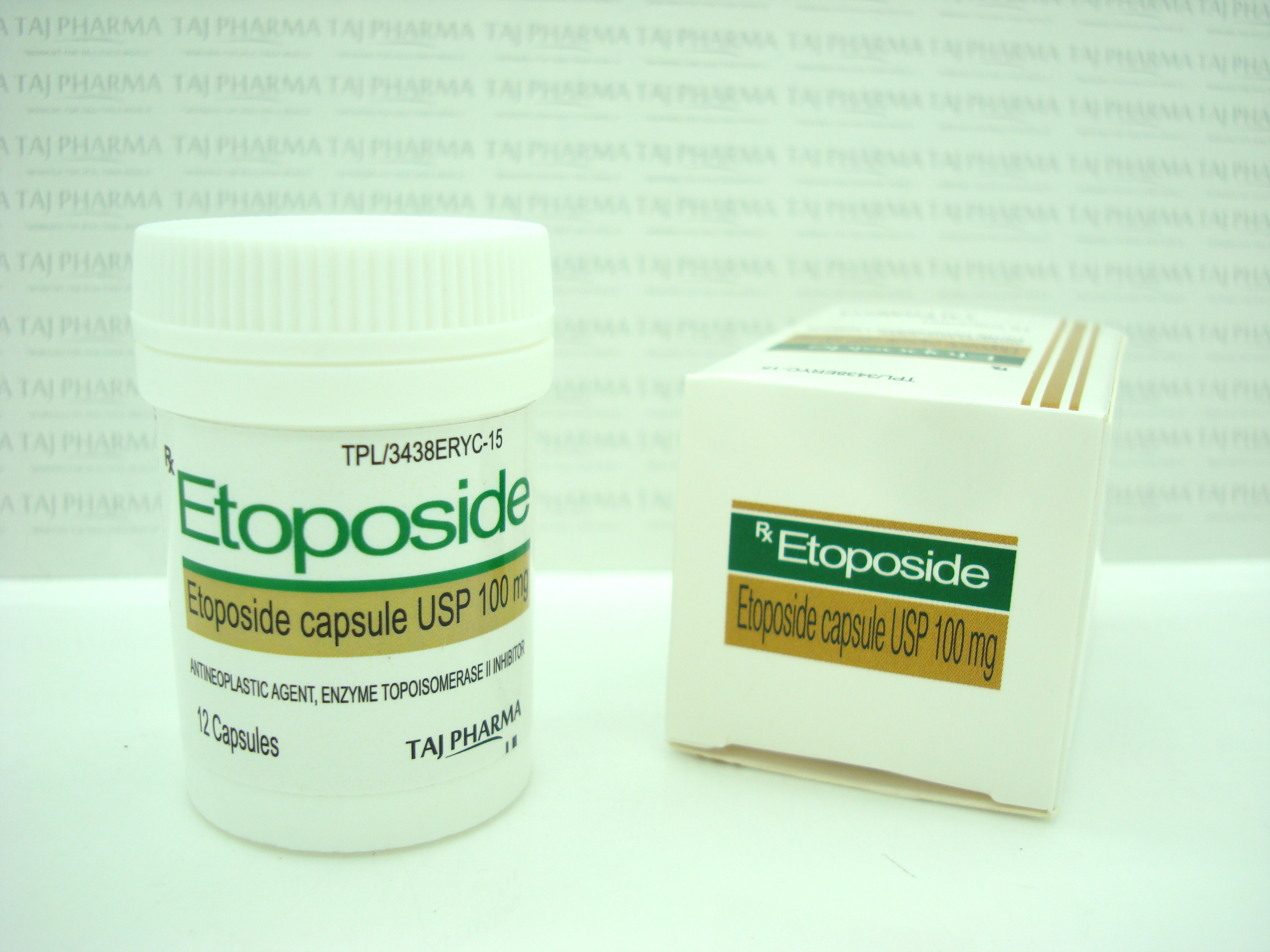
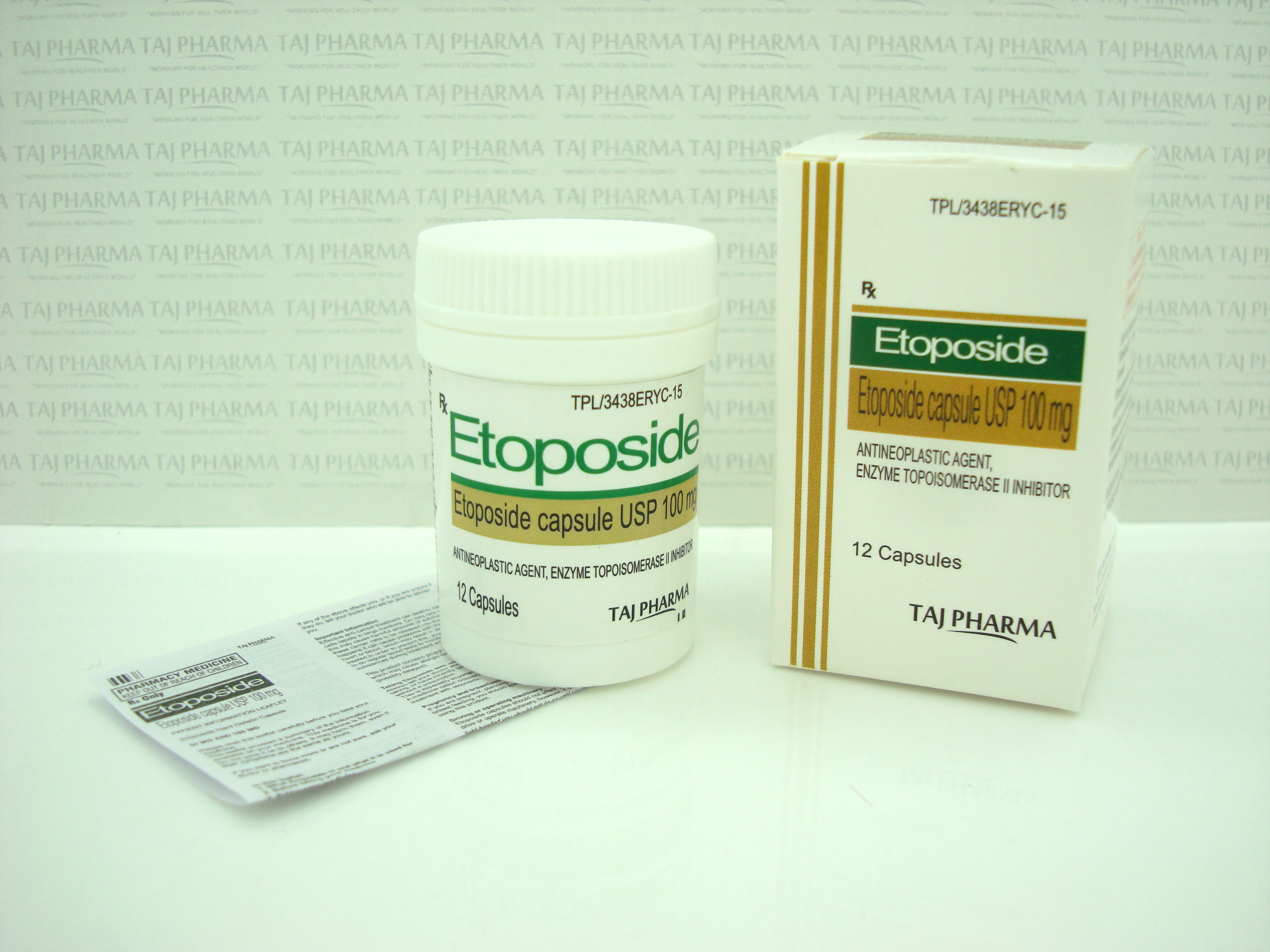
Etoposide
100mg/5ml Injection
Etoposide (also commonly known as VP-16) is a semisynthetic derivative of podophyllotoxin used in the treatment of certain neoplastic diseases. It is 4’-demethylepipodophyllotoxin 9-[4,6-0-(R)-ethylidine-ß-D-glucopyranoside]. It is very soluble in methanol and chloroform, slightly soluble in ethanol, and sparingly soluble in water and ether. It is made more miscible with water by means of organic solvents.
Etoposide Injection, USP is available for intravenous use as a
20 mg/mL solution in 100 mg (5 mL),
500 mg (25 mL), or 1 gram (50 mL) sterile,
multiple dose vials.
The pH of the clear yellow solution is 3 to 4.
Each mL contains 20 mg etoposide, 2 mg citric acid, 30 mg benzyl alcohol, 80 mg polysorbate 80, 650 mg polyethylene glycol 300, and 30.5 percent (v/v) alcohol.
Etoposide Injection, USP in combination therapy with other approved chemotherapeutic agents in patients with refractory testicular tumors who have already received appropriate surgical, chemotherapeutic, and radiotherapeutic therapy.
Etoposide Injection, USP in combination with other approved chemotherapeutic agents as first line treatment in patients with small cell lung cancer.
Etoposide
100mg/5ml Injection
WHAT ETOPOSIDE IS AND WHAT IT IS USED FOR
- The name of this medicine is Etoposide 20 mg/ml Concentrate for solution for infusion. It contains the active ingredient Etoposide. Etoposide belongs to a type of drugs known and podophyllotoxin derivatives and it slows or stops the growth of cancer cells.
- Etoposide is one of the medicines used to treat a variety of cancers. It can be used alone or in combination with other chemotherapeutic agents.
- This medicine is used for the treatment of testicular cancer, lung cancer and certain cases of leukemia (blood cancer).
BEFORE ETOPOSIDE IS GIVEN TO YOU
When Etoposide Should Not be given to you
If the answer is YES to any of these questions, you should probably not receive Etoposide. Please discuss the matter with your doctor immediately.
However, your doctor may decide that your treatment with Etoposide is essential.
- are you allergic to etoposide or to one of the other ingredients of this concentrate?
- do you have problems with your liver?
- do you have severe kidney problems?
- do you have problems with the functioning of the bone marrow?
- is the treatment used for a new born baby?
- are you pregnant or planning to become pregnant (see also "Pregnancy and breastfeeding" below)?
- are you breast feeding?
When special care should be taken
If the answer is YES to any of these questions, it is important that you discuss the matter with your doctor BEFORE receiving your first injection.
- are you using other drugs to treat cancer?
- are you receiving, or did you receive in the past, radiation therapy?
- are you suffering from infections?
Tell your doctor about any other treatment you receive for your illness.
Using other medicines
Please tell your doctor if you are taking or have recently taken any other medicines, including medicines obtained without a prescription.
In particular you should tell your doctor if you are taking any of the following:
- anti-coagulants such as warfarin which are used to thin the blood
- the analgesic (pain killing) and fever lowering medicines phenylbutazone, aspirin and aspirin related medicines (sodium salicylate or salicylic acid)
- the immunosuppressant ciclosporine (often given after an organ transplant)
- other drugs used to treat other forms of cancers such as vinblastine, doxorubicin and cisplatin
Etoposide can also have effects on other medicines used to treat cancer. Your doctor will take these effects into account when deciding on your treatment.
Using Etoposide with food and drink
Etoposide is not affected by food or drink.
Pregnancy and breast-feeding
- You should not use Etoposide if you are pregnant. If you are pregnant you should inform your doctor immediately. Women of child bearing age should take effective contraceptive measures.
You should not breastfeed during treatment with Etoposide.
Fathering children whilst taking Etoposide
- Men should not father a child whilst being treated with Etoposide and until 6 months after treatment has finished. It is advised for men to consider sperm collection (for cryo-conservation) before treatment with etoposide, because infertility after treatment can occur.
Driving and using machines
- This medication can cause nausea and vomiting. Precaution is advised in undertaking actions which require extra alertness, such as the use of machines and driving.
Important information about some of the ingredients of Etoposide
- This medicinal product contains approximately 30% ethanol (alcohol), i.e. up to 1.5 g per dose. This is equivalent to 30 ml of beer or 12.5 ml of wine per dose. This may be dangerous for patients suffering from alcoholism and for patients in high-risk groups such as those with liver problems or epilepsy (fits). The amount of alcohol in this product may alter the effects of other medicines.
- Etoposide contains 30 mg/ml of benzyl alcohol and must not be given to premature babies or new born babies. It may cause toxic and allergic reactions in infants and children up to 3 years old.
HOW ETOPOSIDE IS GIVEN TO YOU
- Etoposide concentrate for solution for infusion will always be given to you by a healthcare professional. This medicine will be diluted with 0.9 % sodium chloride or 5 % dextrose and will be given to you as an infusion (a "drip") into a vein.
How much of the injection will you receive and how often?
- The dose of Etoposide will be individually determined by your doctor. The dose you are given depends on your size: it varies with your surface area. Technically, this is measured in square metres, and is worked out from your height and weight..
- You will receive a treatment cycle consisting of one dose a day during 3 - 5 days, followed by a 10 - 20 days rest.
- The administration will take at least 30 minutes.
- Usually three or four treatment cycles are given, but the duration of the treatment and the number of treatments is determined by the doctor and may vary for each patient.
- Etoposide may be given alone or in combination with other medicines.
- Your condition will be closely monitored during treatment. This routinely involves blood tests and controls of your liver function
- Your dose may be changed depending on your kidney function.
If you have any questions about your treatment schedule ask your doctor, pharmacist or nurse.
If you are given too much Etoposide
If you think you have received too much medicine consult your doctor or a nurse.
If you missed a dose of Etoposide
If you have missed a dose of your treatment, consult your doctor or a nurse.
POSSIBLE SIDE EFFECTS
Like all medicines, Etoposide can cause side effects, although not everybody gets them.
You should discuss them with your doctor who will explain the risks and benefits of your treatment.
Some of the side effects can be lessened or treated by other medicines or therapy.
Tell your doctor immediately if you notice any of the following:
- unexplained bruising, reddish or purplish patches on the skin, nosebleeds and bleeding (these may be signs of a decrease in the number of blood platelets, those cells in the blood that help the blood to clot)
- infections
- severe allergic reactions such as fever, reddening of the face and neck, often with a sudden, subjective feeling of heat (flushing), rapid heartbeat, abnormal contraction of your lungs which can cause a cough and wheezing, abnormally low blood pressure and stopping of breathing.
It may be necessary to stop your treatment with Etoposide.
Although not all of these side effects may occur, tell your doctor if they do occur, as they may need medical attention.
The following headings are used to organise the side effects in order of frequency:
- Very common: (may affect more than 1 in 10 users)
- Common: (may affect 1 to 10 users in 100)
- Uncommon: (may affect 1 to 10 users in 1,000)
- Rare: (may affect 1 to 10 users in 10,000)
- Very rare: (may affect 1 user in 10,000)
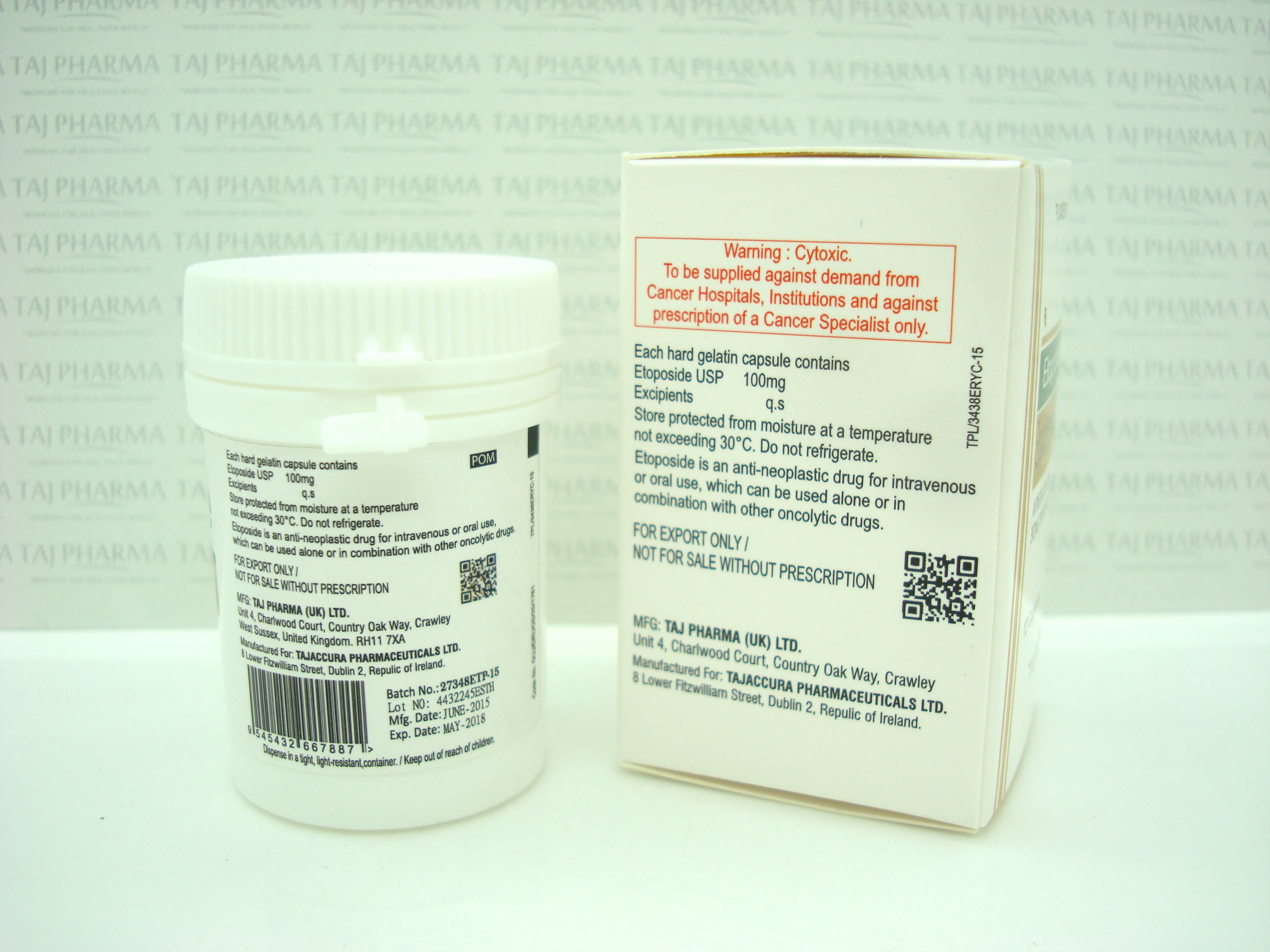
The following information is intended for medical or healthcare professionals only:
Cytotoxic
Instructions on how to dilute, administer, store and dispose of Etoposide
Dilution
- Etoposide 20 mg/ml concentrate for solution for infusion must be diluted immediately prior to use with either 5% dextrose in water, or 0.9% sodium chloride solution to give a final concentration of 0.2 to 0.4 mg/ml. At higher concentrations precipitation of etoposide may occur.
Administration
- The usual dose of etoposide, in combination with other approved chemotherapeutic agents, ranges from 100-120 mg/m²/day via continuous infusion over 30 minutes for 3-5 days, followed by a resting period of 10-20 days.
- Generally 3 to 4 chemotherapy cycles are administered. Dose and amount of cycles should be adjusted to the level of bone marrow suppression and the reaction of the tumour.
- In patients with renal function impairment the dose should be adjusted.
- Etoposide is intended for intravenous administration only.
The SIDE EFFECTS could include:
Very Common side effects
- you may produce less red blood cells (anaemia) and platelets than normal. This will be monitored by your doctor during your treatment with regular blood tests.
- infections
- nausea
- vomiting
- loss of appetite
- reversible loss of hair (alopecia), sometimes progressing to total baldness
- feeling of tiredness due to anaemia
Common Side Effects
- leukaemia (cancer of the blood) in addition to the cancer that you are being treated for bleeding
- allergic (hypersensitive) reactions such as fever, reddening of the face and neck, often with a sudden, subjective feeling of heat (flushing), rapid heartbeat, abnormal contraction of your lungs which can cause a cough and wheezing, abnormally low blood pressure and stopping of breathing
- redness of the skin
- facial and tongue swelling
- coughing
- sweating
- bluish discoloration of the skin and mucous membranes
- convulsions (fits)
- spasmodic closure of the voice box (larynx)
- abnormally high blood pressure
- fatigue and drowsiness
- low blood pressure causing dizziness when Etoposide is adminsitered too quickly
- abominal pain
- diarrhoea
- inflammation of the mucous membrane of the mouth
- problems with your liver including increase in liver blood test values (bilirubin, SGOT and alkaline phosphatases); your doctor will monitor your liver function with blood tests during your treatment
Uncommon side effects
- damage to nerves of the hand and feet
- irregular heartbeat
- heartattack
- abnormal contractions in your lungs which can cause a cough and wheezing
- coughing
- spasmodic closure of your throat which makes it difficult to breath-in.
- inflammation of the mucous membranes
- inflammation of the gullet (oesophagus)
- rash
- hives
- darkening of skin (increase in pigmentation)
- itching
Rare side effects
- allergic (hypersensitive) reactions caused by benzyl alcohol
- stroke, occasionally in association with allergic reactions
- a feeling of weakness
- sensations such as burning, prickling, itching, or tingling
- reversible loss of vision
- temporary blindness
- inflammation of an optic nerve
- unusually high concentration of uric acid in the blood (gout)
- inflammation of a vein
- when you are receiving the infusion, if it leaks into the surrounding tissues then irritation and swelling may occur around the location of the leakage
- stopping breathing
- inflammation of the tissue in the lungs
- formation of scar tissue in the lungs
- constipation
- difficulty in swallowing
- taste impairment
- Etoposide can accumulate in your liver and kidneys, especially if you have liver or kidney problems
Very rare side effects
- a potentially life-threatening skin disorder accompanied by severe skin blisters and often sores in the membrains of the mouth, nose, eyes and the anal and gential areas.
- inflammatory, itching skin reddening following radiation therapy and subsequent treatment with a rash at the site of previous radiotherapy
- redness and pain of palms of hands and soles of feet
If any of the side effects gets serious, or if you notice any side effects not listed in this leaflet, please tell your doctor.
HOW TO STORE ETOPOSIDE
- Keep out of the reach and sight of children.
- Do not use Etoposide after the expiry date which is stated on the vial and carton after EXP. The expiry date refers to the last day of that month.
- Keep the vial in the outer carton, in order to protect from light. Do not refrigerate or freeze.
- After dilution the solution should be used immediately. If this is not possible, the diluted solution may be stored at 15 – 25 ° C for not more than 12 hours.
- Avoid unnecessary contact with the fluid. Rinse skin immediately after contact with the solution. Be sure your doctor or nurse removes any syringes or vials for disposal.
FURTHER INFORMATION
What Etoposide contains
- The active substanceis Etoposide. Each vial (5ml) contains 100 mg Etoposide
- The other ingredients are benzyl alcohol, citric acid, ethanol, polysorbate 80 and macrogol 300.
What Etoposide looks like and contents of the pack
- Etoposide Concentrate for solution for infusion is a clear to pale yellow solution packaged in clear glass vials containing 5 ml of solution. The vials are packed in carton boxes containing 1 or 10 vials.
Not all pack sizes may be marketed.
To prevent the occurrence of hypotension, the infusion should be given over at least 30 minutes.
Storage of the prepared solution
- Chemical and physical in-use stability has been demonstrated for 24 hours 15-25 °C.
- From a microbiological point of view, the diluted product should be used immediately. If not used immediately, in-use storage times and conditions prior to use are the responsibility of the user and would normally not be longer than 12 hours at 15 – 25 °C, unless dilution has taken place in controlled and validated aseptic conditions.
Handling and disposal
The normal procedures for proper handling and disposal of anti-tumour medicinal products should be adopted:
- Staff should be trained to reconstitute the medicinal product.
- Pregnant staff should be excluded from working with this medicinal product.
- Staff handling this medicinal product during reconstitution should wear protective clothing including mask, goggles and gloves.
- All items for administration or cleaning, including gloves, should be placed in high-risk, waste disposal bags for high-temperature incineration.
- Liquid waste may be flushed with large amounts of water.
- Accidental contact with the skin or eyes should be treated immediately with copious amounts of water.
Etoposide
100mg/5ml Injection
DESCRIPTION
Etoposide (also commonly known as VP-16) is a semisynthetic derivative of podophyllotoxin used in the treatment of certain neoplastic diseases. It is 4’-demethylepipodophyllotoxin 9-[4,6-0-(R)-ethylidine-ß-D-glucopyranoside]. It is very soluble in methanol and chloroform, slightly soluble in ethanol, and sparingly soluble in water and ether. It is made more miscible with water by means of organic solvents.
Etoposide Injection, USP is available for intravenous use as a 20 mg/mL solution in 100 mg (5 mL), 500 mg (25 mL), or 1 gram (50 mL) sterile, multiple dose vials. The pH of the clear yellow solution is 3 to 4. Each mL contains 20 mg etoposide, 2 mg citric acid, 30 mg benzyl alcohol, 80 mg polysorbate 80, 650 mg polyethylene glycol 300, and 30.5 percent (v/v) alcohol. The structural formula is:

C29H32O13 M.W. 588.56
CLINICAL PHARMACOLOGY
Etoposide has been shown to cause metaphase arrest in chick fibroblasts. Its main effect, however, appears to be at the G2 portion of the cell cycle in mammalian cells. Two different dose-dependent responses are seen. At high concentrations (10 mcg/mL or more), lysis of cells entering mitosis is observed. At low concentrations (0.3 to 10 mcg/mL), cells are inhibited from entering prophase. It does not interfere with microtubular assembly. The predominant macromolecular effect of etoposide appears to be the induction of DNA strand breaks by an interaction with DNA topoisomerase II or the formation of free radicals.
Pharmacokinetics
On intravenous administration, the disposition of etoposide is best described as a biphasic process with a distribution half-life of about 1.5 hours and terminal elimination half-life ranging from 4 to 11 hours. Total body clearance values range from 33 to 48 mL/min or 16 to 36 mL/min/m2 and, like the terminal elimination half-life, are independent of dose over a range 100 to 600 mg/m2. Over the same dose range, the areas under the plasma concentration vs time curves (AUC) and the maximum plasma concentration (Cmax) values increase linearly with dose. Etoposide does not accumulate in the plasma following daily administration of 100 mg/m2 for 4 to 5 days.
The mean volumes of distribution at steady state fall in the range of 18 to 29 liters or 7 to 17 L/m2. Etoposide enters the CSF poorly. Although it is detectable in CSF and intracerebral tumors, the concentrations are lower than in extracerebral tumors and in plasma. Etoposide concentrations are higher in normal lung than in lung metastases and are similar in primary tumors and normal tissues of the myometrium. In vitro, etoposide is highly protein bound (97%) to human plasma proteins. An inverse relationship between plasma albumin levels and etoposide renal clearance is found in children. In a study determining the effect of other therapeutic agents on the in vitro binding of carbon-14 labeled etoposide to human serum proteins, only phenylbutazone, sodium salicylate, and aspirin displaced protein-bound etoposide at concentrations achieved in vivo.1
Etoposide binding ratio correlates directly with serum albumin in patients with cancer and in normal volunteers. The unbound fraction of etoposide significantly correlated with bilirubin in a population of cancer patients.2 Data have suggested a significant inverse correlation between serum albumin concentration and free fraction of etoposide.
After intravenous administration of 3H-etoposide (70 to 290 mg/m2), mean recoveries of radioactivity in the urine range from 42 to 67%, and fecal recoveries range from 0 to 16% of the dose. Less than 50% of an intravenous dose is excreted in the urine as etoposide with mean recoveries of 8 to 35% within 24 hours.
In children, approximately 55% of the dose is excreted in the urine as etoposide in 24 hours. The mean renal clearance of etoposide is 7 to 10 mL/min/m2 or about 35% of the total body clearance over a dose range of 80 to 600 mg/m2. Etoposide, therefore, is cleared by both renal and nonrenal processes, i.e., metabolism and biliary excretion. The effect of renal disease on plasma etoposide clearance is not known.
Biliary excretion appears to be a minor route of etoposide elimination. Only 6% or less of an intravenous dose is recovered in the bile as etoposide. Metabolism accounts for most of the nonrenal clearance of etoposide. The major urinary metabolite of etoposide in adults and children is the hydroxy acid [4’-demethylepipodophyllic acid-9-(4,6-0-(R)-ethylidene-ß-D-glucopyranoside)], formed by opening of the lactone ring. It is also present in human plasma, presumably as the trans isomer. Glucuronide and/or sulfate conjugates of etoposide are excreted in human urine and represent 5 to 22% of the dose. In addition, O-demethylation of the dimethoxyphenol ring occurs through the CYP450 3A4 isoenzyme pathway to produce the corresponding catechol.
After intravenous infusion, the Cmax and AUC values exhibit marked intra- and inter-subject variability.
In adults, the total body clearance of etoposide is correlated with creatinine clearance, serum albumin concentration, and nonrenal clearance. Patients with impaired renal function receiving etoposide have exhibited reduced total body clearance, increased AUC and a lower volume of distribution at steady state. Use of cisplatin therapy is associated with reduced total body clearance. In children, elevated serum SGPT levels are associated with reduced drug total body clearance. Prior use of cisplatin may also result in a decrease of etoposide total body clearance in children.
Although some minor differences in pharmacokinetic parameters between age and gender have been observed, these differences were not considered clinically significant.
INDICATIONS AND USAGE
Etoposide Injection, USP is indicated in the management of the following neoplasms:
Refractory Testicular Tumors
Etoposide Injection, USP in combination therapy with other approved chemotherapeutic agents in patients with refractory testicular tumors who have already received appropriate surgical, chemotherapeutic, and radiotherapeutic therapy.
Small Cell Lung Cancer
Etoposide Injection, USP in combination with other approved chemotherapeutic agents as first line treatment in patients with small cell lung cancer.
CONTRAINDICATIONS
Etoposide Injection, USP is contraindicated in patients who have demonstrated a previous hypersensitivity to etoposide or any component of the formulation.
WARNINGS
Patients being treated with etoposide must be frequently observed for myelosuppression both during and after therapy. Myelosuppression resulting in death has been reported. Dose-limiting bone marrow suppression is the most significant toxicity associated with etoposide therapy. Therefore, the following studies should be obtained at the start of therapy and prior to each subsequent cycle of etoposide: platelet count, hemoglobin, white blood cell count and differential. The occurrence of a platelet count below 50,000/mm3 or an absolute neutrophil count below 500/mm3 is an indication to withhold further therapy until the blood counts have sufficiently recovered.
Physicians should be aware of the possible occurrence of an anaphylactic reaction manifested by chills, fever, tachycardia, bronchospasm, dyspnea, and hypotension. Higher rates of anaphylactic-like reactions have been reported in children who received infusions at concentrations higher than those recommended. The role that concentration of infusion (or rate of infusion) plays in the development of anaphylactic-like reactions is uncertain. Treatment is symptomatic. The infusion should be terminated immediately, followed by the administration of pressor agents, corticosteroids, antihistamines, or volume expanders at the discretion of the physician.
Etoposide Injection, USP should be given only by slow intravenous infusion (usually over a 30 to 60 minute period) since hypotension has been reported as a possible side effect of rapid intravenous injection.
Pregnancy
Etoposide can cause fetal harm when administered to a pregnant woman. Etoposide has been shown to be teratogenic in mice and rats.
In rats, an intravenous etoposide dose of 0.4 mg/kg/day (about 1/20th of the human dose on a mg/m2 basis) during organogenesis caused maternal toxicity, embryotoxicity, and teratogenicity (skeletal abnormalities, exencephaly, encephalocele, and anophthalmia); higher doses of 1.2 and 3.6 mg/kg/day (about 1/7th and 1/2 of human dose on a mg/m2 basis) resulted in 90 and 100% embryonic resorptions. In mice, a single 1 mg/kg (1/16th of human dose on a mg/m2 basis) dose of etoposide administered intraperitoneally on days 6, 7, or 8 of gestation caused embryotoxicity, cranial abnormalities, and major skeletal malformations. An I.P. dose of 1.5 mg/kg (about 1/10th of human dose on a mg/m2 basis) on day 7 of gestation caused an increase in the incidence of intrauterine death and fetal malformations and a significant decrease in the average fetal body weight.
Women of childbearing potential should be advised to avoid becoming pregnant. If this drug is used during pregnancy, or if the patient becomes pregnant while receiving this drug, the patient should be warned of the potential hazard to the fetus.
Etoposide should be considered a potential carcinogen in humans. The occurrence of acute leukemia with or without a preleukemic phase has been reported in rare instances in patients treated with etoposide alone or in association with other neoplastic agents. The risk of development of a preleukemic or leukemic syndrome is unclear. Carcinogenicity tests with etoposide have not been conducted in laboratory animals.
PRECAUTIONS
General
In all instances where the use of etoposide is considered for chemotherapy, the physician must evaluate the need and usefulness of the drug against the risk of adverse reactions. Most such adverse reactions are reversible if detected early. If severe reactions occur, the drug should be reduced in dosage or discontinued and appropriate corrective measures should be taken according to the clinical judgment of the physician. Reinstitution of etoposide therapy should be carried out with caution, and with adequate consideration of the further need for the drug and alertness as to possible recurrence of toxicity.
Patients with low serum albumin may be at an increased risk for etoposide associated toxicities.
Laboratory Tests
Periodic complete blood counts should be done during the course of etoposide treatment. They should be performed prior to each cycle of therapy and at appropriate intervals during and after therapy. At least one determination should be done prior to each dose of etoposide.
Renal Impairment
In patients with impaired renal function, the following initial dose modification should be considered based on measured creatinine clearance:
| Measured Creatinine Clearance | > 50 mL/min | 15-50 mL/min |
| etoposide | 100% of dose | 75% of dose |
Subsequent etoposide dosing should be based on patient tolerance and clinical effect.
Data are not available in patients with creatinine clearances <15 mL/min and further dose reduction should be considered in these patients.
Carcinogenesis, (see WARNINGS), Mutagenesis, Impairment of Fertility
Etoposide has been shown to be mutagenic in Ames assay.
Treatment of Swiss-Albino mice with 1.5 mg/kg I.P. of etoposide on day 7 of gestation increased the incidence of intrauterine death and fetal malformations as well as significantly decreased the average fetal body weight. Maternal weight gain was not affected.
Irreversible testicular atrophy was present in rats treated with etoposide intravenously for 30 days at 0.5 mg/kg/day (about 1/16th of the human dose on a mg/m2 basis).
Pregnancy
Pregnancy Category D.
See WARNINGS.
Nursing Mothers
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from etoposide, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
Etoposide Injection, USP contains polysorbate 80. In premature infants, a life-threatening syndrome consisting of liver and renal failure, pulmonary deterioration, thrombocytopenia, and ascites has been associated with an injectable vitamin E product containing polysorbate 80. Anaphylactic reactions have been reported in pediatric patients.
Drug Interactions
High-dose cyclosporine resulting in concentrations above 2000 ng/mL administered with oral etoposide has led to an 80% increase in etoposide exposure with a 38% decrease in total body clearance of etoposide compared to etoposide alone.
ADVERSE REACTIONS
The following data on adverse reactions are based on both oral and intravenous administration of etoposide as a single agent, using several different dose schedules for treatment of a wide variety of malignancies.
Hematologic Toxicity
Myelosuppression is dose related and dose limiting, with granulocyte nadirs occurring 7 to 14 days after drug administration and platelet nadirs occurring 9 to 16 days after drug administration. Bone marrow recovery is usually complete by day 20, and no cumulative toxicity has been reported. Fever and infection have also been reported in patients with neutropenia. Death associated with myelosuppression has been reported.
The occurrence of acute leukemia with or without a preleukemic phase has been reported rarely in patients treated with etoposide in association with other antineoplastic agents.
Gastrointestingal Toxicity
Nausea and vomiting are the major gastrointestinal toxicities. The severity of such nausea and vomiting is generally mild to moderate with treatment discontinuation required in 1% of patients. Nausea and vomiting can usually be controlled with standard antiemetic therapy. Mild to severe mucositis/esophagitis may occur. Gastrointestinal toxicities are slightly more frequent after oral administration than after intravenous infusion.
Hypotension
Transient hypotension following rapid intravenous administration has been reported in 1% to 2% of patients. It has not been associated with cardiac toxicity or electrocardiographic changes. No delayed hypotension has been noted. To prevent this rare occurrence, it is recommended that etoposide be administered by slow intravenous infusion over a 30 to 60 minute period. If hypotension occurs, it usually responds to cessation of the infusion and administration of fluids or other supportive therapy as appropriate. When restarting the infusion, a slower administration rate should be used.
Allergic Reactions
Anaphylactic-like reactions characterized by chills, fever, tachycardia, bronchospasm, dyspnea and/or hypotension have been reported to occur in 0.7% to 2% of patients receiving intravenous etoposide and in less than 1% of the patients treated with the oral capsules. These reactions have usually responded promptly to the cessation of the infusion and administration of pressor agents, corticosteroids, antihistamines, or volume expanders as appropriate; however, the reactions can be fatal. Hypertension and/or flushing have also been reported. Blood pressure usually normalizes within a few hours after cessation of the infusion. Anaphylactic-like reactions have occurred during the initial infusion of etoposide.
Facial/tongue swelling, coughing, diaphoresis, cyanosis, tightness in throat, laryngospasm, back pain and/or loss of consciousness have sometimes occurred in association with the above reactions. In addition, an apparent hypersensitivity-associated apnea has been reported rarely.
Rash, urticaria, and/or pruritus have infrequently been reported at recommended doses. At investigational doses, a generalized pruritic erythematous maculopapular rash, consistent with perivasculitis, has been reported.
Alopecia
Reversible alopecia, sometimes progressing to total baldness, was observed in up to 66% of patients.
Other Toxicities
The following adverse reactions have been infrequently reported: abdominal pain, aftertaste, constipation, dysphagia, asthenia, fatigue, malaise, somnolence, transient cortical blindness, optic neuritis, interstitial pneumonitis/pulmonary fibrosis, fever, seizure, (occasionally associated with allergic reactions), Stevens-Johnson syndrome, and toxic epidermal necrolysis, pigmentation, and a single report of radiation recall dermatitis.
Hepatic toxicity, generally in patients receiving higher doses of the drug than those recommended, has been reported with etoposide. Metabolic acidosis has also been reported in patients receiving higher doses.
Reports of extravasation with swelling have been received postmarketing. Rarely extravasation has been associated with necrosis and venous induration.
The incidences of adverse reactions in the table that follows are derived from multiple data bases from studies in 2,081 patients when etoposide was used either orally or by injection as a single agent.
| ADVERSE DRUG EFFECT | PERCENT RANGE OF REPORTED INCIDENCE |
|---|---|
| Hematologic toxicity | |
| Leukopenia (less than 1,000 WBC/mm3) | 3 to 17 |
| Leukopenia (less than 4,000 WBC/mm3) | 60 to 91 |
| Thrombocytopenia (less than 50,000 platelets/mm3) | 1 to 20 |
| Thrombocytopenia (less than 100,000 platelets/mm3) | 22 to 41 |
| Anemia | 0 to 33 |
| Gastrointestinal toxicity | |
| Nausea and vomiting | 31 to 43 |
| Abdominal pain | 0 to 2 |
| Anorexia | 10 to 13 |
| Diarrhea | 1 to 13 |
| Stomatitis | 1 to 6 |
| Hepatic | 0 to 3 |
| Alopecia | 8 to 66 |
| Peripheral neurotoxicity | 1 to 2 |
| Hypotension | 1 to 2 |
| Allergic reaction | 1 to 2 |
OVERDOSAGE
No proven antidotes have been established for etoposide overdosage.
DOSAGE AND ADMINISTRATION
Note: Plastic devices made of acrylic or ABS (a polymer composed of acrylonitrile, butadiene, and styrene) have been reported to crack and leak when used with undiluted Etoposide Injection, USP.
The usual dose of Etoposide Injection, USP in testicular cancer in combination with other approved chemotherapeutic agents ranges from 50 to 100 mg/m2/day on days 1 through 5 to 100 mg/m2/day on days 1, 3, and 5.
In small cell lung cancer, the Etoposide Injection, USP dose in combination with other approved chemotherapeutic drugs ranges from 35 mg/m2/day for 4 days to 50 mg/m2/day for 5 days.
For recommended dosing adjustments in patients with renal impairment.
Chemotherapy courses are repeated at 3- to 4-week intervals after adequate recovery from any toxicity.
The dosage, by either route, should be modified to take into account the myelosuppressive effects of other drugs in the combination or the effects of prior x-ray therapy or chemotherapy which may have compromised bone marrow reserve.
Administration Precautions
As with other potentially toxic compounds, caution should be exercised in handling and preparing the solution of etoposide. Skin reactions associated with accidental exposure to etoposide may occur. The use of gloves is recommended. If etoposide solution contacts the skin or mucosa, immediately and thoroughly wash the skin with soap and water and flush the mucosa with water.
Preparation for Intravenous Administration
Etoposide Injection, USP must be diluted prior to use with either 5% Dextrose Injection, USP, or 0.9% Sodium Chloride Injection, USP, to give a final concentration of 0.2 to 0.4 mg/mL. If solutions are prepared at concentrations above 0.4 mg/mL, precipitation may occur. Hypotension following rapid intravenous administration has been reported, hence, it is recommended that the etoposide solution be administered over a 30- to 60-minute period. A longer duration of administration may be used if the volume of fluid to be infused is a concern. Etoposide should not be given by rapid intravenous injection.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit.
Stability
nopened vials of Etoposide Injection, USP are stable for 24 months at room temperature (25°C). Vials diluted as recommended to a concentration of 0.2 or 0.4 mg/mL are stable for 96 and 24 hours, respectively, at room temperature (25°C) under normal room fluorescent light in both glass and plastic containers.
Procedures for proper handling and disposal of anticancer drugs should be considered. Several guidelines on this subject have been published4-10. There is no general agreement that all of the procedures recommended in the guidelines are necessary or appropriate.
HOW SUPPLIED
Etoposide Injection, USP is supplied as follows:
| 20 mg/mL in a 5 mL, sterile multiple dose vial, individually boxed in a package of 10. |
| 20 mg/mL in a 25 mL, sterile multiple dose vial, individually boxed. |
| 20 mg/mL in a 50 mL, sterile multiple dose vial, individually boxed. |
Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature].
Vial stoppers do not contain natural rubber latex.
REFERENCES
- Gaver RC; Deeb G; “The effect of other drugs on the in vitro binding of 14C-etoposide to human serum proteins.” Proc Am Assoc Cancer Res; 30:A2132, 1989.
- Stewart CF; Pieper JA; Arbuck SG; Evans WE; “Altered protein binding of etoposide in patients with cancer.” Clin Pharmacol Ther; 45:49-55 1989.
- Stewart CF; Arbuck SG; Fleming RA; Evans WE; “Prospective evaluation of a model for predicting etoposide plasma protein binding in cancer patients.” Proc Am Assoc Cancer Res; 30:A958, 1989.
- Recommendations for the Safe Handling of Parenteral Antineoplastic Drugs, NIH Publication No. 83-2621. For sale by the Superintendent of Documents, US Government Printing Office, Washington, D.C. 20402.
- AMA Council Report. Guidelines for Handling Parenteral Antineoplastics. JAMA. 1985; 253 (11): 1590-1592.
- National Study Commission on cytotoxic Exposure - Recommendations for Handling Cytotoxic Agents. Available from Louis P. Jeffrey, Sc.D., Chairman, National Study Commission on Cytotoxic Exposure, Massachusetts College of Pharmacy and Allied Health Sciences, 179 Longwood Avenue, Boston, Massachusetts 02115.
- Clinical Oncological Society of Australia. Guidelines and Recommendations for Safe Handling of Antineoplastic Agents. Med J Australia 1983; 1:426-428.
- Jones RB, et al; Safe handling of chemotherapeutic agents: A report from the Mount Sinai Medical Center. CA-A Cancer Journal for Clinicians. 1983; (Sept/Oct) 258-263.
- American Society of Hospital Pharmacists Technical Assistance Bulletin on Handling Cytotoxic and Hazardous Drugs. Am J Hosp Pharm 1990; 47:1033-1049.
- Controlling occupational exposure to hazardous drugs. (OSHA WORK PRACTICE GUIDELINES). Am J Health-Syst Pharm 1996; 53:1669-1685.
Product Glimpse
Description
We are committed to work towards a healthier and happier world. The company is an integrated, research based international pharmaceutical company, producing a wide range of quality, affordable generic (Etoposide 100mg/5ml Injection) medicines, trusted by health-care professionals and patients across geographies.
We offer you the highest quality new Generic medicines ie. Etoposide 100mg/5ml Injection, drugs and also with innovative packing at the lowest prices shipped to you from India. Browse our latest Pharmaceuticals and Generics possibilities and other pharmaceuticals possibilities…more.