Dacarbazine 100mg/200mg Injection
Dacarbazine
200mg Injection
Dacarbazine for Injection per vial as sterile dacarbazine packaged in individual cartons.
Store in a refrigerator 2°C to 8°C (36°F to 46°F).
Dacarbazine for Injection is indicated in the treatment of metastatic malignant melanoma. In addition, Dacarbazine for Injection is also indicated for Hodgkin’s disease as a second-line therapy when used in combination with other effective agents.
Dacarbazine for Injection is a colorless to an ivory colored solid which is light sensitive. Each vial contains 200 mg of dacarbazine (the active ingredient), citric acid monohydrate and mannitol.
WARNING
It is recommended that Dacarbazine for Injection be administered under the supervision of a qualified physician experienced in the use of cancer chemotherapeutic agents.
Hemopoietic depression is the most common toxicity with Dacarbazine for Injection (see WARNINGS).
Hepatic necrosis has been reported (see WARNINGS).
Studies have demonstrated this agent to have a carcinogenic and teratogenic effect when used in animals.
In treatment of each patient, the physician must weigh carefully the possibility of achieving therapeutic benefit against the risk of toxicity.
Dacarbazine
200mg Injection
What Dacarbazine is and what it is used for
Dacarbazine Powder for Solution for Injection is an anti-cancer medicine, in the form of a powder for
solution for injection. Treatment with an anti-cancer medicine is sometimes called cancer chemotherapy.
Dacarbazine Powder for Solution for Injection may be used for the treatment of some types of cancer, for example: metastatic malignant melanoma (a type of skin cancer that has spread) and Hodgkin’s disease and some types of cancer in soft tissues.
Before you use Dacarbazine
Do not use Dacarbazine Powder for Solution for Injection- if you have shown signs of hypersensitivity (severe allergy) to dacarbazine on previous occasions
- if you have severe liver or kidney diseases
- in combination with yellow fever vaccine.
- if you are pregnant, trying to become pregnant or are breast feeding
Special care should be taken if you are taking other medicinal products which could interact with Dacarbazine:
- ciclosporin or tacrolimus (medicines used after having a transplant)
- fotemustine (a medicine used in cancer treatment)
- medicines which could damage your liver
- warfarin (a medicine used to thin the blood). Your doctor may need to do your blood test (INR) more often.
Please tell your doctor if you are taking, or have recently taken, any other medicines, including medicines obtained without a prescription.
Taking with Food and DrinkYou should avoid alcohol while receiving chemotherapy treatment with dacarbazine
Pregnancy and breast feedingDo not use Dacarbazine:
- if you are pregnant or trying to become pregnant
- if you are breast feeding
Dacarbazine may influence the ability to drive or operate machinery because of nausea and vomiting or rare adverse reactions affecting the nervous system.
Important information about one of the ingredients of Dacarbazine Powder for Solution for InjectionThis medicine contains less than 1 mmol sodium (23 mg) per vial, i.e. essentially ‘sodium free’.
How to use Dacarbazine
This medicinal product is for intravenous use (injection into a vein).
Your treatment will usually be given to you in hospital.
You will be given dacarbazine as an infusion (slow injection via a drip) into a vein or a slow intravenous
injection (injection into a vein).
Tell your doctor or nurse at once if you notice any pain at the injection site during or shortly after treatment.
Pain around the injection site could mean the needle has not been properly inserted into the vein.
The dose of dacarbazine will depend on the illness for which you are being treated. The dose is calculated
according to your body surface area (expressed as mg/m2).
Depending on your illness, dosing is typically between 200 and 850 mg/m2 of dacarbazine.
As this medicine will be given to you whilst you are in hospital it is unlikely that you will be given too little
or too much. However, tell your doctor or pharmacist if you have any concerns.
Possible Side Effects
Like all medicines Dacarbazine Powder for Solution for Injection can have side effects although not everybody gets them.
If any of the following happen, tell your doctor immediately:
severe allergic reaction - you may experience a sudden itchy rash (hives), swelling of the hands, feet, ankles, face, lips, mouth and throat (which may cause difficulty in swallowing or breathing), and you may feel you are going to faint.
This is a very serious side effect. You may need urgent medical attention. This very serious side effect is rare.
If you experience any of the following tell your doctor as soon as possible:
Common (less than 1 in 10 patients but more than 1 in 100):
blood problems: they are dependent on how strong your dose is and are more likely after 3 to 4 weeks.
You may feel tired, look pale, bruise more easily than usual or get more infections than usual. They are shown by blood tests:
- decreased red blood cells (anaemia)
- decreased white blood cells (leukopenia)
- decreased platelets (thrombocytopenia)
- decreased formation of all blood cells in the bone marrow (bone marrow suppression)
- loss of appetite
- nausea/vomiting
Uncommon (Less than 1 in 100 patients but more than 1 in 1000):
- confusion
- fits (seizures)
- numbness of the skin or pins and needles sensation in the face (paraesthesia)
- headache
- blurred vision
- facial flushing
- hair loss (alopecia)
- transient rash
- an influenza (‘flu’) type syndrome of fever, muscle pain (myalgia) and generally feeling unwell
- (malaise) which may start approximately one week after treatment and may last for up to three weeks
- tiredness and weakness (lethargy)
- abnormal kidney and liver function (shown in tests)
- liver damage (hepatotoxicity)
- blockage of a vein in your liver (also called Budd-Chiari syndrome) resulting in liver tissue damage (necrosis), in some cases even to death. The signs include fever, stomach pain and yellow eyes and skin (jaundice). Your doctor would also be able to see that your liver was larger and you would have changes in the numbers of your blood cells.
Rare (less than 1 in 1000 patients but more than 1 in 10,000)
- diarrhoea
- irritation at the injection site
- increased sensitivity of the skin to sunlight (photosensitivity)
Very rare (less than 1 in 10,000)
- swelling of the face, lips, mouth and throat with difficulty breathing (anaphylactic reactions)
- redness of the skin (erythema)
- rash with spots and blisters (maculopapular exanthema)
- nettle rash (urticaria)
- itching
Blood samples will be taken to check for changes in blood cells levels. Blood and urine tests will be
performed to check for changes in kidney function. Blood tests may be performed to check that your liver is
working properly.
If any of the side effects gets serious, or if you notice any side effects not listed in this leaflet, please tell your
doctor.
How to store Dacarbazine
Keep out of the reach and sight of children
The vials should be stored at 2 - 8°C with the vials kept in the outer carton (in order to protect from light).
This medicine should not be used after the expiry date printed on the vial label.
Further Information
What Dacarbazine Powder for Solution for Injection contains
The medicine is presented in glass containers called vials containing 200 mg dacarbazine. Each pack contains 1 vial.
- The active substance is dacarbazine
- The other ingredients are citric acid monohydrate, mannitol and sodium hydroxide
What Dacarbazine Powder for Solution for Injection looks like and contents of the pack
The powder is a white or pale yellow solid.
The vial containing the powder is a glass container with a rubber stopper.
Each single-dose vial contains 200 mg of Dacarbazine. When reconstituted each ml of solution contains 10 mg of dacarbazine.
The 200 mg presentation of dacarabazine is sold in packs containing 1 vial of powder
Dacarbazine
200mg Injection
WARNING
It is recommended that Dacarbazine for Injection be administered under the supervision of a qualified physician experienced in the use of cancer chemotherapeutic agents.
- Hemopoietic depression is the most common toxicity with Dacarbazine for Injection
- Hepatic necrosis has been reported
- Studies have demonstrated this agent to have a carcinogenic and teratogenic effect when used in animals.
- In treatment of each patient, the physician must weigh carefully the possibility of achieving therapeutic benefit against the risk of toxicity.
DESCRIPTION
Dacarbazine for Injection is a colorless to an ivory colored solid which is light sensitive. Each vial contains 200 mg of dacarbazine (the active ingredient), citric acid monohydrate and mannitol. Dacarbazine for Injection is reconstituted and administered intravenously (pH 3-4). Dacarbazine is an anticancer agent designated chemically as 5-(3,3-dimethyl-1-triazeno)-imidazole-4-carboxamide with the following structural formula:

CLINICAL PHARMACOLOGY
After intravenous administration of Dacarbazine for Injection, the volume of distribution exceeds total body water content suggesting localization in some body tissue, probably the liver. Its disappearance from the plasma is biphasic with initial half-life of 19 minutes and a terminal half-life of 5 hours. In a patient with renal and hepatic dysfunctions, the half-lives were lengthened to 55 minutes and 7.2 hours. The average cumulative excretion of unchanged dacarbazine in the urine is 40% of the injected dose in 6 hours. Dacarbazine is subject to renal tubular secretion rather than glomerular filtration. At therapeutic concentrations dacarbazine is not appreciably bound to human plasma protein.
In man, dacarbazine is extensively degraded. Besides unchanged dacarbazine, 5-aminoimidazole−4−carboxamide (AIC) is a major metabolite of dacarbazine excreted in the urine. AIC is not derived endogenously but from the injected dacarbazine, because the administration of radioactive dacarbazine labeled with 14C in the imidazole portion of the molecule (dacarbazine-2-14C) gives rise to AIC-2-14C.
Although the exact mechanism of action of Dacarbazine for Injection is not known, three hypotheses have been offered:
- inhibition of DNA synthesis by acting as a purine analog
- action as an alkylating agent
- interaction with SH groups
INDICATIONS AND USAGE
Dacarbazine for Injection is indicated in the treatment of metastatic malignant melanoma. In addition, Dacarbazine for Injection is also indicated for Hodgkin’s disease as a second-line therapy when used in combination with other effective agents.
CONTRAINDICATIONS
Dacarbazine for Injection is contraindicated in patients who have demonstrated a hypersensitivity to it in the past.
WARNINGS
Hemopoietic depression is the most common toxicity with Dacarbazine for Injection and involves primarily the leukocytes and platelets, although, anemia may sometimes occur. Leukopenia and thrombocytopenia may be severe enough to cause death. The possible bone marrow depression requires careful monitoring of white blood cells, red blood cells and platelet levels. Hemopoietic toxicity may warrant temporary suspension or cessation of therapy with Dacarbazine for Injection.
Hepatic toxicity accompanied by hepatic vein thrombosis and hepatocellular necrosis resulting in death, has been reported. The incidence of such reactions has been low; approximately 0.01% of patients treated. This toxicity has been observed mostly when Dacarbazine for Injection has been administered concomitantly with other anti-neoplastic drugs: however, it has also been reported in some patients treated with Dacarbazine for Injection alone.
Anaphylaxis can occur following the administration of Dacarbazine for Injection.
PRECAUTIONS
Hospitalization is not always necessary but adequate laboratory study capability must be available. Extravasation of the drug subcutaneously during intravenous administration may result in tissue damage and severe pain. Local pain, burning sensation and irritation at the site of injection may be relieved by locally applied hot packs.
Carcinogenicity of dacarbazine was studied in rats and mice. Proliferative endocardial lesions, including fibrosarcomas and sarcomas were induced by dacarbazine in rats. In mice, administration of dacarbazine resulted in the induction of angiosarcomas of the spleen.
USAGE IN PREGNANCY
Pregnancy Category C:
Dacarbazine for Injection has been shown to be teratogenic in rats when given in doses 20 times the human daily dose on day 12 of gestation. Dacarbazine when administered in 10 times the human daily dose to male rats (twice weekly for 9 weeks) did not affect the male libido, although female rats mated to male rats had higher incidence of resorptions than controls. In rabbits, dacarbazine daily dose 7 times the human daily dose given on Days 6 − 15 of gestation resulted in fetal skeletal anomalies. There are no adequate and well controlled studies in pregnant women. Dacarbazine for Injection should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for tumorigenicity shown for Dacarbazine for Injection in animal studies, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
ADVERSE REACTIONS
Symptoms of anorexia, nausea and vomiting are the most frequently noted of all toxic reactions. Over 90% of patients are affected with the initial few doses. The vomiting lasts 1 − 12 hours and is incompletely and unpredictably palliated with phenobarbital and/or prochlorperazine. Rarely, intractable nausea and vomiting have necessitated discontinuance of therapy with Dacarbazine for Injection. Rarely, Dacarbazine for Injection has caused diarrhea. Some helpful suggestions include restricting the patient’s oral intake of food for 4 − 6 hours prior to treatment. The rapid toleration of these symptoms suggests that a central nervous system mechanism may be involved, and usually these symptoms subside after the first 1 or 2 days.
There are a number of minor toxicities that are infrequently noted. Patients have experienced an influenza-like syndrome of fever to 39°C, myalgias and malaise. These symptoms occur usually after large single doses, may last for several days, and they may occur with successive treatments.
Alopecia has been noted as has facial flushing and facial paresthesia. There have been few reports of significant liver or renal function test abnormalities in man. However, these abnormalities have been observed more frequently in animal studies.
Erythematous and urticarial rashes have been observed infrequently after administration of Dacarbazine for Injection. Rarely, photosensitivity reactions may occur.
OVERDOSAGE
Give supportive treatment and monitor blood cell counts.
DOSAGE AND ADMINISTRATION
Malignant Melanoma:
The recommended dosage is 2 to 4.5 mg/kg/day for 10 days. Treatment may be repeated at 4 week intervals.
An alternate recommended dosage is 250 mg/square meter body surface/day IV for 5 days. Treatment may be repeated every 3 weeks.
Hodgkin's Disease:
The recommended dosage of Dacarbazine for Injection in the treatment of Hodgkin’s disease is 150 mg/square meter body surface/day for 5 days, in combination with other effective drugs. Treatment may be repeated every 4 weeks. An alternative recommended dosage is 375 mg/square meter body surface on day 1, in combination with other effective drugs, to be repeated every 15 days.
Dacarbazine for Injection 200 mg/vial is reconstituted with 19.7 mL of Sterile Water for Injection, USP. The resulting solution contains 10 mg/mL of dacarbazine having a pH of 3.0 to 4.0. The calculated dose of the resulting solution is drawn into a syringe and administered only intravenously.
The reconstituted solution may be further diluted with 5% dextrose injection, USP or sodium chloride injection, USP and administered as an intravenous infusion.
After reconstitution and prior to use, the solution in the vial may be stored at 4°C for up to 72 hours or at normal room conditions (temperature and light) for up to 8 hours. If the reconstituted solution is further diluted in 5% dextrose injection, USP or sodium chloride injection, USP, the resulting solution may be stored at 4°C for up to 24 hours or at normal room conditions for up to 8 hours.
Procedures for proper handling and disposal of anticancer drugs should be considered. Several guidelines on this subject have been published1-7. There is no general agreement that all the procedures recommended in the guidelines are necessary or appropriate.
HOW SUPPLIED
200 mg of Dacarbazine for Injection per vial as sterile dacarbazine packaged in individual cartons.
STORAGE CONDITIONS
Store in a refrigerator 2°C to 8°C (36°F to 46°F).
REFERENCES
- Recommendations for the Safe Handling of Parenteral Antineoplastic Drugs. NIH Publication No. 83 − 2621. For sale by the Superintendent of Documents, U.S. Government Printing Office, Washington, D.C., 20402.
- AMA Council Report. Guidelines for Handling Parenteral Antineoplastics. JAMA, March 15, 1985.
- National Study Commission on Cytotoxic Exposure − Recommendations for Handling Cytotoxic Agents. Available from Louis P. Jeffrey, Sc. D., Director of Pharmacy Services, Rhode Island Hospital, 593 Eddy Street, Providence, Rhode Island, 02902.
- Clinical Oncological Society of Australia: Guidelines and recommendations for safe handling of antineoplastic agents. Med. J. Australia 1. 426-428, 1983.
- Jones, R. B., et al., Safe handling of chemotherapeutic agents: A report from the Mount Sinai Medical Center. Ca-A Cancer Journal for Clinicians Sept./Oct., 258-263. 1983.
- American Society of Hospital Pharmacists technical assistance bulletin on handling cytotoxic drugs in hospitals. Am. J. Hosp. Pharm. 42: 131-137, 1985.
- OSHA Work-Practice Guidelines for Personnel Dealing with Cytotoxic (Antineoplastic) Drugs. Am J Hosp Pharm 1986; 43: 1193-1204.
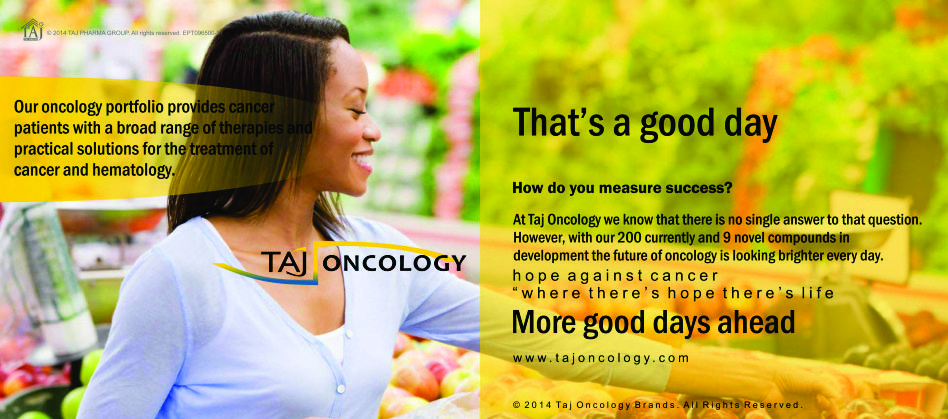
Product Glimpse
Description
We are committed to work towards a healthier and happier world. The company is an integrated, research based international pharmaceutical company, producing a wide range of quality, affordable generic (Dacarbazine 100mg/200mg Injection) medicines, trusted by health-care professionals and patients across geographies.
We offer you the highest quality new Generic medicines ie. Dacarbazine 100mg/200mg Injection, drugs and also with innovative packing at the lowest prices shipped to you from India. Browse our latest Pharmaceuticals and Generics possibilities and other pharmaceuticals possibilities…more.