Azathioprine 100mg Injection
Azathioprine
Azathioprine 100mg Injection
Azathioprine Sodium for Injection, USP, is supplied in a 20 mL vial, each containing azathioprine sodium, equivalent to 100 mg azathioprine.
Store at 20° to 25°C (68° to 77°F).
Protect from light. Retain in carton until time of use.
The sterile, lyophilized sodium salt is yellow, and should be dissolved in Sterile Water for Injection
Azathioprine Sodium for Injection, USP is a sterile lyophilized material, which when reconstituted with Sterile Water for Injection yields a solution for intravenous administration. Each vial contains azathioprine sodium equivalent to 100 mg azathioprine, an immunosuppressive antimetabolite. Each vial also contains sodium hydroxide and, if necessary, hydrochloric acid to adjust the pH.
It is an imidazolyl derivative of 6-mercaptopurine and many of its biological effects are similar to those of the parent compound.
Azathioprine is insoluble in water, but may be dissolved with addition of one molar equivalent of alkali. The sodium salt of azathioprine is sufficiently soluble to make a 10 mg/mL water solution which is stable for 24 hours at 59° to 77°F (15° to 25°C). Azathioprine is stable in solution at neutral or acid pH but hydrolysis to mercaptopurine occurs in excess sodium hydroxide (0.1N), especially on warming. Conversion to mercaptopurine also occurs in the presence of sulfhydryl compounds such as cysteine, glutathione and hydrogen sulfide.
Azathioprine 100mg Injection
What Azathioprine is and what it is used for
Azathioprine injection contains a medicine called azathioprine. This belongs to a group of medicines called immunosuppressants. These medicines reduce the activity of your body's immune system.
Azathioprine is used to:
- stop your body rejecting an organ transplant
- treat diseases where your immune system reacts against your own body (called autoimmune diseases, such as rheumatoid arthritis).
Ask your doctor, nurse or pharmacist if you would like any further explanation about these uses.
Before you have Azathioprine
Do not have Azathioprine if:
you are allergic (hypersensitive) to azathioprine, mercaptopurine or any of the other ingredients of Azathioprine (listed in section 6).
Azathioprine Sodium 100mg Injection and different pharma Tablet & Capsule formulations are also available in different drug delivery forms. We also have large volume manufacturing facilities for these Products.
If you are not sure, talk to your doctor, nurse or pharmacist before having Azathioprine.
Take special care with Azathioprine
Check with your doctor, nurse or pharmacist before having Azathioprine if:
- you have liver or kidney disease
- you have 'Lesch-Nyhan Syndrome'. This is a rare condition that runs in families caused by a lack of something called HPRT or 'hypoxanthine-guanine-phosphoribosyltransferase'
- you have a condition where your body produces too little of something called TPMT or 'thiopurine methyltransferase'
- you have ever suffered from chickenpox or shingles.
If you are not sure if any of the above apply to you, talk to your doctor, nurse or pharmacist before having Azathioprine .
Taking other medicines
Please tell your doctor, nurse or pharmacist if you are taking or have recently taken any other medicines. This includes medicines obtained without a prescription, including herbal medicines. This is because Azathioprine can affect the way some medicines work. Also some other medicines can affect the way Azathioprine works.
In particular, tell your doctor, nurse or pharmacist if you are taking any of the following medicines:
- allopurinol - used for gout
- tubocurarine or succinylcholine - used during operations
- warfarin - used for blood dots
- penicillamine - used for rheumatoid arthritis
- co-trimoxazole - used for infections
- captopril - used for high blood pressure or heart problems
- cimetidine - used for stomach ulcers and indigestion
- indomethacin - used for pain and inflammation
- furosemide - used for high blood pressure and heart problems
- olsalazine or mesalazine - used for a bowel problem called ulcerative colitis
- sulfasalzine or balsalazide - used for rheumatoid arthritis or ulcerative colitis.
If you are not sure if any of the above apply to you, talk to your doctor, nurse or pharmacist before having Azathioprine.
Having vaccines while you are using Azathioprine
If you are going to have a vaccination speak to your doctor or nurse before you have it. This is because vaccines may not work properly while you are having Azathioprine.
Tests you may have while having Azathioprine
Your doctor may ask you to have a blood test while you are having Azathioprine . This is to check your blood cell count. Your doctor may change your dose of Azathioprine after the test.
Trying for a baby, pregnancy and breast-feeding
- Do not have Azathioprine if you are a man trying to have a baby. This is because it may affect the baby.
- Do not have Azathioprine if you are a woman who is pregnant or think you might become pregnant. This is because it may affect the baby.
- Do not have Azathioprine if you are breast-feeding. This is because small amounts may pass into the mother's milk.
Ask your doctor, midwife or pharmacist for advice before taking any medicine, if you are pregnant or breast-feeding.
Azathioprine and the sun
While having Azathioprine you may be more likely to develop some types of cancers such as skin cancer. Some people also become sensitive to sunlight which can cause skin discolouration or a rash. Take care to avoid too much sun, cover up and use sunscreen.
Chickenpox/Shingles infection
Infection with chickenpox or shingles can become severe in patients taking immunosuppressive medicine. Therefore you should avoid contact with anyone suffering from chickenpox or shingles.
Important information about some of the ingredients of Azathioprine Injection
Azathioprine injection contains sodium. Each 50 mg vial contains 4.5 mg of sodium. If you are on a low sodium diet, talk to your doctor, nurse or pharmacist before you have Azathioprine.
How to take Azathioprine
The dose of Azathioprine you have depends on your illness and how bad it is. The dose also depends on your age, your weight and how well your liver and kidneys are working. Your doctor will explain this to you.
To stop your body rejecting an organ transplant
On the first day
- the usual dose is up to 5 mg per kg of body weight.
For the rest of your treatment
- you will have between 1 and 4 mg per kg of body weight each day.
For other conditions
At the start of your treatment
- you will have 1 to 3 mg per kg of body weight each day
- your doctor may reduce your dose later.
If you have more Azathioprine than you should
Your doctor will give you Azathioprine so it is unlikely that you will receive too much. If you think you have been given too much or have missed a dose, tell your doctor or nurse.
Possible side effects
Like all medicines, Azathioprine can cause side effects, although not everybody gets them.
The following side effects may happen with this medicine:
If you notice any of the following serious side effects, talk to your specialist doctor or go to hospital straight away:
- allergic reaction, the signs may include:
- general tiredness, dizziness, feeling sick (nausea), being sick (vomiting) or diarrhoea
- high temperature (fever), shivering or chills
- redness of the skin or a skin rash
- pain in the muscles or joints
- changes in the amount and colour of the urine (kidney problems)
- dizziness, confusion, feeling light headed or weak, caused by low blood pressure
- you bruise more easily or notice any unusual bleeding
- you have a high temperature (fever) or other signs of an infection
- you feel extremely tired
- you notice lumps anywhere on your body
- you notice any changes to your skin, for example blisters or peeling
- your health suddenly gets worse
- you come into contact with anyone who is suffering from chickenpox or shingles.
If you notice any of the above, stop having Azathioprine and see a doctor straight away.
Other side effects include:
Very common (affects more than 1 in 10 people)
- infections caused by a virus, fungus or bacteria
- reduction in your bone marrow function, which may make you feel unwell or show up in your blood tests
- low white blood cell level in your blood tests, which may cause an infection.
Common (affects less than 1 in 10 people)
- low blood platelet level, which may cause you to bruise or bleed easily.
Uncommon (affects less than 1 in 100 people)
- low red blood cell level, which may cause you to be tired, get headaches, be short of breath when exercising, feel dizzy and look pale
- inflammation of the pancreas, which may cause you severe upper stomach pain, with feeling sick (nausea) and being sick (vomiting)
- liver problems, which may cause pale stools, dark urine, itchiness and yellowing of your skin and eyes.
Rare (affects less than 1 in 1,000 people)
- problems with your blood and bone marrow which may cause weakness, tiredness, paleness, headaches, sore tongue, breathlessness, bruising or infections
- problems with your bowel leading to diarrhoea, abdominal pain, constipation, feeling sick (nausea) and being sick (vomiting)
- hair loss which may get better even though you continue to take Azathioprine
- severe liver damage which can be life-threatening
- various types of cancers including blood, lymph and skin cancers
- sensitivity to sunlight which can cause skin discolouration or a rash.
Very rare (affects less than 1 in 10,000 people)
- inflammation of your lungs causing breathlessness, cough and a fever.
If any of the side effects gets serious, or if you notice any other side effects not listed in this leaflet, please tell your doctor, nurse or pharmacist.
How to store Azathioprine
- Do not store above 25°C.
- Protect from light and keep dry.
- Keep out of the reach and sight of children.
- Do not use Azathioprine after the expiry date which is stated on the label. The expiry date refers to the last day of that month.
- Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. These measures will help to protect the environment.
AZATHIOPRINE SODIUM
FOR INJECTION
Rx ONLY
DESCRIPTION
Azathioprine Sodium for Injection, USP is a sterile lyophilized material, which when reconstituted with Sterile Water for Injection yields a solution for intravenous administration. Each vial contains azathioprine sodium equivalent to 100 mg azathioprine, an immunosuppressive antimetabolite. Each vial also contains sodium hydroxide and, if necessary, hydrochloric acid to adjust the pH.
Azathioprine is chemically 6-[(1-methyl-4-nitroimidazol-5-yl)thio]purine. The structural formula of azathioprine sodium is:

Molecular Formula: C9H7N7O2SNa Molecular Weight: 300.28
It is an imidazolyl derivative of 6-mercaptopurine and many of its biological effects are similar to those of the parent compound.
Azathioprine is insoluble in water, but may be dissolved with addition of one molar equivalent of alkali. The sodium salt of azathioprine is sufficiently soluble to make a 10 mg/mL water solution which is stable for 24 hours at 59° to 77°F (15° to 25°C). Azathioprine is stable in solution at neutral or acid pH but hydrolysis to mercaptopurine occurs in excess sodium hydroxide (0.1N), especially on warming. Conversion to mercaptopurine also occurs in the presence of sulfhydryl compounds such as cysteine, glutathione and hydrogen sulfide.
CLINICAL PHARMACOLOGY
Azathioprine is well absorbed following oral administration. Maximum serum radioactivity occurs at 1 to 2 hours after oral 35S-azathioprine and decays with a half-life of 5 hours. This is not an estimate of the half-life of azathioprine itself, but is the decay rate for all 35S-containing metabolites of the drug. Because of extensive metabolism, only a fraction of the radioactivity is present as azathioprine. Usual doses produce blood levels of azathioprine, and of mercaptopurine derived from it, which are low (<1 mcg/mL). Blood levels are of little predictive value for therapy since the magnitude and duration of clinical effects correlate with thiopurine nucleotide levels in tissues rather than with plasma drug levels. Azathioprine and mercaptopurine are moderately bound to serum proteins (30%) and are partially dialyzable.
Azathioprine is metabolized to 6-mercaptopurine (6-MP). Both compounds are rapidly eliminated from blood and are oxidized or methylated in erythrocytes and liver; no azathioprine or mercaptopurine is detectable in urine after 8 hours. Activation of 6-mercaptopurine occurs via hypoxanthine-guanine phosphoribosyltransferase (HGPRT) and a series of multi-enzymatic processes involving kinases to form 6-thioguanine nucleotides (6TGNs) as major metabolites. The cytotoxicity of azathioprine is due, in part, to the incorporation of 6-TGN into DNA.
6-MP undergoes two major inactivation routes. One is thiol methylation, which is catalyzed by the enzyme thiopurine S-methyltransferase (TPMT), to form the inactive metabolite methyl-6-MP (6-MeMP). TPMT activity is controlled by a genetic polymorphism. 1,2,3 For Caucasians and African Americans, approximately 10% of the population inherit one non-functional TPMT allele (heterozygous) conferring intermediate TPMT activity, and 0.3% inherit two TPMT non-functional alleles (homozygous) for low or absent TPMT activity. Non-functional alleles are less common in Asians. TPMT activity correlates inversely with 6TGN levels in erythrocytes and presumably other hematopoietic tissues, since these cells have negligible xanthine oxidase (involved in the other inactivation pathway) activities, leaving TPMT methylation as the only inactivation pathway. Patients with intermediate TPMT activity may be at increased risk of myelotoxicity if receiving conventional doses of azathioprine. Patients with low or absent TPMT activity are at an increased risk of developing severe, life-threatening myelotoxicity if receiving conventional doses of azathioprine.4-9 TPMT genotyping or phenotyping (red blood cell TPMT activity) can help identify patients who are at an increased risk for developing azathioprine toxicity.2, 3, 7, 8, 9 Accurate phenotyping (red blood cell TPMT activity) results are not possible in patients who have received recent blood transfusions.
Figure 1. Metabolism pathway of azathioprine : competing pathways result in inactivation by TPMT or XO, or incorporation of cytotoxic nucleotides into DNA.

GMPS: Guanosine monophosphate synthetase; HGPRT: Hypoxanthine-guanine-phosphoribosyl-transferase; IMPD: Inosine monophosphate dehydrogenase; MeMP: Methylmercaptopurine; MeMPN: Methylmercaptopurine nucleotide; TGN: Thioguanine nucleotides; TIMP: Thioinosine monophosphate; TPMT: Thiopurine S-methyltransferase; TU Thiouric acid; XO: Xanthine oxidase (Adapted from Pharmacogenomics 2002; 3:89-98; and Cancer Res 2001; 61:5810-5816.)
Another inactivation pathway is oxidation, which is catalyzed by xanthine oxidase (XO) to form 6-thiouric acid. The inhibition of xanthine oxidase in patients receiving allopurinol is the basis for the azathioprine dosage reduction required in these patients. Proportions of metabolites are different in individual patients, and this presumably accounts for variable magnitude and duration of drug effects. Renal clearance is probably not important in predicting biological effectiveness or toxicities, although dose reduction is practiced in patients with poor renal function.
Homograft Survival
The use of azathioprine for inhibition of renal homograft rejection is well established, the mechanism(s) for this action are somewhat obscure. The drug suppresses hypersensitivities of the cell-mediated type and causes variable alterations in antibody production. Suppression of T-cell effects, including ablation of T-cell suppression, is dependent on the temporal relationship to antigenic stimulus or engraftment. This agent has little effect on established graft rejections or secondary responses.
Alterations in specific immune responses or immunologic functions in transplant recipients are difficult to relate specifically to immunosuppression by azathioprine. These patients have subnormal responses to vaccines, low numbers of T-cells, and abnormal phagocytosis by peripheral blood cells, but their mitogenic responses, serum immunoglobulins and secondary antibody responses are usually normal.
Immunoinflammatory Response
Azathioprine suppresses disease manifestations as well as underlying pathology in animal models of auto-immune disease. For example, the severity of adjuvant arthritis is reduced by azathioprine.
The mechanisms whereby azathioprine affects autoimmune diseases are not known. Azathioprine is immunosuppressive, delayed hypersensitivity and cellular cytotoxicity tests being suppressed to a greater degree than are antibody responses. In the rat model of adjuvant arthritis, azathioprine has been shown to inhibit the lymph node hyperplasia which precedes the onset of the signs of the disease. Both the immunosuppressive and therapeutic effects in animal models are dose-related. Azathioprine is considered a slow-acting drug and effects may persist after the drug has been discontinued.
INDICATIONS AND USAGE
Azathioprine Sodium for Injection, USP is indicated as an adjunct for the prevention of rejection in renal homotransplantation. It is also indicated for the management of active rheumatoid arthritis to reduce signs and symptoms.
Renal Homotransplantation
Azathioprine is indicated as an adjunct for the prevention of rejection in renal homotransplantation. Experience with over 16,000 transplants shows a five-year patient survival of 35% to 55%, but this is dependent on donor, match for HLA antigens, anti-donor or anti-B-cell alloantigen antibody and other variables. The effect of azathioprine on these variables has not been tested in controlled trials.
Rheumatoid Arthritis
Azathioprine is indicated for the treatment of active rheumatoid arthritis (RA) to reduce signs and symptoms. Aspirin, non-steroidal anti-inflammatory drugs and/or low dose glucocorticoids may be continued during treatment with azathioprine. The combined use of azathioprine with disease modifying anti-rheumatic drugs (DMARDs) has not been studied for either added benefit or unexpected adverse effects. The use of azathioprine with these agents cannot be recommended.
CONTRAINDICATIONS
Azathioprine Sodium for Injection should not be given to patients who have shown hypersensitivity to the drug. Azathioprine should not be used for treating rheumatoid arthritis in pregnant women. Patients with rheumatoid arthritis previously treated with alkylating agents (cyclophosphamide, chlorambucil, melphalan or others) may have a prohibitive risk of malignancy if treated with azathioprine.
WARNINGS
Malignancy:
Patients receiving immunosuppressants, including azathioprine, are at increased risk of developing lymphoma and other malignancies, particularly of the skin. Physicians should inform patients of the risk of malignancy with azathioprine. As usual for patients with increased risk for skin cancer, exposure to sunlight and ultraviolet light should be limited by wearing protective clothing and using a sunscreen with a high protection factor.
Post-transplant:
Renal transplant patients are known to have an increased risk of malignancy, predominantly skin cancer and reticulum cell or lymphomatous tumors. The risk of post-transplant lymphomas may be increased in patients who receive aggressive treatment with immunosuppressive drugs, including azathioprine. Therefore, immunosuppressive drug therapy should be maintained at the lowest effective levels.
Rheumatoid Arthritis:
Information is available on the risk of malignancy with the use of azathioprine in rheumatoid arthritis. It has not been possible to define the precise risk of malignancy due to azathioprine. The data suggest the risk may be elevated in patients with rheumatoid arthritis, though lower than for renal transplant patients. However, acute myelogenous leukemia as well as solid tumors have been reported in patients with rheumatoid arthritis who have received azathioprine.
Inflammatory Bowel Disease:
Postmarketing cases of hepatosplenic T-cell lymphoma (HSTCL), a rare type of T-cell lymphoma, have been reported in patients treated with azathioprine. These cases have had a very aggressive disease course and have been fatal. The majority of reported cases have occurred in patients with Crohn's disease or ulcerative colitis and the majority were in adolescent and young adult males. Some of the patients were treated with azathioprine as monotherapy and some had received concomitant treatment with a TNFα blocker at or prior to diagnosis. The safety and efficacy of azathioprine for the treatment of Crohn's disease and ulcerative colitis have not been established.
Cytopenias:
Severe leukopenia, thrombocytopenia, anemias including macrocytic anemia, and/or pancytopenia may occur in patients being treated with azathioprine. Severe bone marrow suppression may also occur. Patients with intermediate thiopurine S-methyl transferase (TPMT) activity may be at an increased risk of myelotoxicity if receiving conventional doses of azathioprine. Patients with low or absent TPMT activity are at an increased risk of developing severe, life-threatening myelotoxicity if receiving conventional doses of azathioprine. TPMT genotyping or phenotyping can help identify patients who are at an increased risk for developing azathioprine toxicity. Hematologic toxicities are dose-related and may be more severe in renal transplant patients whose homograft is undergoing rejection. It is suggested that patients on azathioprine have complete blood counts, including platelet counts, weekly during the first month, twice monthly for the second and third months of treatment, then monthly or more frequently if dosage alterations or other therapy changes are necessary. Delayed hematologic suppression may occur. Prompt reduction in dosage or temporary withdrawal of the drug may be necessary if there is a rapid fall in or persistently low leukocyte count, or other evidence of bone marrow depression. Leukopenia does not correlate with therapeutic effect; therefore the dose should not be increased intentionally to lower the white blood cell count.
Serious infections:
Patients receiving immunosuppressants, including azathioprine, are at increased risk for bacterial, viral, fungal, protozoal, and opportunistic infections, including reactivation of latent infections. These infections may lead to serious, including fatal, outcomes.
Progressive Multifocal Leukoencephalopathy
Cases of JC virus-associated infection resulting in progressive multifocal leukoencephalopathy (PML), sometimes fatal, have been reported in patients treated with immunosuppressants, including azathioprine. Risk factors for PML include treatment with immunosuppressant therapies and impairment of immune function. Consider the diagnosis of PML in any patient presenting with new-onset neurological manifestations and consider consultation with a neurologist as clinically indicated. Consider reducing the amount of immunosuppression in patients who develop PML. In transplant patients, consider the risk that the reduced immunosuppression represents to the graft.
Effect on Sperm in Animals:
Azathioprine has been reported to cause temporary depression in spermatogenesis and reduction in sperm viability and sperm count in mice at doses 10 times the human therapeutic dose;10 a reduced percentage of fertile matings occurred when animals received 5 mg/kg. 11
Pregnancy: Pregnancy Category D
Azathioprine can cause fetal harm when administered to a pregnant woman. Azathioprine should not be given during pregnancy without careful weighing of risk versus benefit. Whenever possible, use of azathioprine in pregnant patients should be avoided. This drug should not be used for treating rheumatoid arthritis in pregnant women.12
Azathioprine is teratogenic in rabbits and mice when given in doses equivalent to the human dose (5 mg/kg daily). Abnormalities included skeletal malformations and visceral anomalies.11
Limited immunologic and other abnormalities have occurred in a few infants born of renal allograft recipients on azathioprine. In a detailed case report,13 documented lymphopenia, diminished IgG and IgM levels, CMV infection, and a decreased thymic shadow were noted in an infant born to a mother receiving 150 mg azathioprine and 30 mg prednisone daily throughout pregnancy. At ten weeks most features were normalized. DeWitte et al reported pancytopenia and severe immune deficiency in a preterm infant whose mother received 125 mg azathioprine and 12.5 mg prednisone daily14. There have been two published reports of abnormal physical findings. Williamson and Karp described an infant born with preaxial polydactyly whose mother received azathioprine 200 mg daily and prednisone 20 mg every other day during pregnancy15. Tallent et al described an infant with a large myelomeningocele in the upper lumbar region, bilateral dislocated hips, and bilateral talipes equinovarus. The father was on long-term azathioprine therapy16.
Benefit versus risk must be weighed carefully before use of azathioprine in patients of reproductive potential. There are no adequate and well-controlled studies in pregnant women. If this drug is used during pregnancy or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus. Women of childbearing age should be advised to avoid becoming pregnant.
PRECAUTIONS
General
A gastrointestinal hypersensitivity reaction characterized by severe nausea and vomiting has been reported. These symptoms may also be accompanied by diarrhea, rash, fever, malaise, myalgias, elevations in liver enzymes, and occasionally, hypotension. Symptoms of gastrointestinal toxicity most often develop within the first several weeks of therapy with azathioprine and are reversible upon discontinuation of the drug. The reaction can recur within hours after re-challenge with a single dose of azathioprine.
Information for Patients
Patients being started on azathioprine should be informed of the necessity of periodic blood counts while they are receiving the drug and should be encouraged to report any unusual bleeding or bruising to their physician. They should be informed of the danger of infection while receiving azathioprine and asked to report signs and symptoms of infection to their physician. Careful dosage instructions should be given to the patient, especially when azathioprine is being administered in the presence of impaired renal function or concomitantly with allopurinol. Patients should be advised of the potential risks of the use of azathioprine during pregnancy and during the nursing period. The increased risk of malignancy following therapy with azathioprine should be explained to the patient.
Laboratory Tests
Complete Blood Count (CBC) Monitoring: Patients on azathioprine should have complete blood counts, including platelet counts, weekly during the first month, twice monthly for the second and third months of treatment, then monthly or more frequently if dosage alterations or other therapy changes are necessary.
TPMT Testing: It is recommended that consideration be given to either genotype or phenotype patients for TPMT. Phenotyping and genotyping methods are commercially available. The most common non-functional alleles associated with reduced levels of TPMT activity are TPMT*2, TPMT*3A and TPMT*3C. Patients with two non-functional alleles (homozygous) have low or absent TPMT activity and those with one non-functional allele (heterozygous) have intermediate activity. Accurate phenotyping (red blood cell TPMT activity) results are not possible in patients who have received recent blood transfusions. TPMT testing may also be considered in patients with abnormal CBC results that do not respond to dose reduction. Early drug discontinuation in these patients is advisable. TPMT TESTING CANNOT SUBSTITUTE FOR COMPLETE BLOOD COUNT (CBC) MONITORING IN PATIENTS RECEIVING AZATHIOPRINE.
Drug Interactions
Use with Allopurinol: One of the pathways for inactivation of azathioprine is inhibited by allopurinol. Patients receiving azathioprine and allopurinol concomitantly should have a dose reduction of azathioprine, to approximately 1/3 to 1/4 the usual dose. It is recommended that a further dose reduction or alternative therapies be considered for patients with low or absent TPMT activity receiving azathioprine and allopurinol because both TPMT and XO inactivation pathways are affected.
Use with Aminosalicylates: There is in vitro evidence that aminosalicylate derivatives (e.g., sulphasalazine, mesalazine, or olsalazine) inhibit the TPMT enzyme. Concomitant use of these agents with azathioprine should be done with caution.
Use with Other Agents Affecting Myelopoesis
Drugs which may affect leukocyte production, including co-trimoxazole, may lead to exaggerated leukopenia, especially in renal transplant recipients.
Use with Angiotensin-Converting Enzyme Inhibitors
The use of angiotensin-converting enzyme inhibitors to control hypertension in patients on azathioprine has been reported to induce anemia and severe leukopenia.
Use with Warfarin
Azathioprine may inhibit the anticoagulant effect of warfarin.
Use with Ribavirin
The use of ribavirin for hepatitis C in patients receiving azathioprine has been reported to induce severe pancytopenia and may increase the risk of azathioprine-related myelotoxicity. Inosine monophosphate dehydrogenase (IMDH) is required for one of the metabolic pathways of azathioprine. Ribavirin is known to inhibit IMDH, thereby leading to accumulation of an azathioprine metabolite, 6-methylthioionosine monophosphate (6-MTITP), which is associated with myelotoxicity (neutropenia, thrombocytopenia, and anemia). Patients receiving azathioprine with ribavirin should have complete blood counts, including platelet counts, monitored weekly for the first month, twice monthly for the second and third months of treatment, then monthly or more frequently if dosage or other therapy changes are necessary.
Carcinogenesis, Mutagenesis, Impairment of Fertility
See WARNINGS section.
Pregnancy
Teratogenic Effects: Pregnancy Category D
See WARNINGS section.
Nursing Mothers
The use of azathioprine in nursing mothers is not recommended. Azathioprine or its metabolites are transferred at low levels, both transplacentally and in breast milk.17,18,19 Because of the potential for tumorigenicity shown for azathioprine, a decision should be made whether to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
Safety and efficacy of azathioprine in pediatric patients have not been established.
ADVERSE REACTIONS
The principal and potentially serious toxic effects of azathioprine are hematologic and gastrointestinal. The risks of secondary infection and malignancy are also significant. The frequency and severity of adverse reactions depend on the dose and duration of azathioprine as well as on the patient’s underlying disease or concomitant therapies. The incidence of hematologic toxicities and neoplasia encountered in groups of renal homograft recipients is significantly higher than that in studies employing azathioprine for rheumatoid arthritis. The relative incidences in clinical studies are summarized below:
|
||
| Toxicity | Renal Homograft | Rheumatoid Arthritis |
|---|---|---|
| Leukopenia | ||
| Any Degree | >50% | 28% |
| <2500 cells/mm3 | 16% | 5.3% |
| Infections | 20% | <1% |
| Neoplasia | * | |
| Lymphoma | 0.5% | |
| Others | 2.8% | |
Hematologic
Leukopenia and/or thrombocytopenia are dose-dependent and may occur late in the course of therapy with azathioprine. Dose reduction or temporary withdrawal may result in reversal of these toxicities. Infection may occur as a secondary manifestation of bone marrow suppression or leukopenia, but the incidence of infection in renal homotransplantation is 30 to 60 times that in rheumatoid arthritis. Anemias, including macrocytic anemia and/or bleeding have been reported.
TPMT genotyping or phenotyping can help identify patients with low or absent TPMT activity (homozygous for non-functional alleles) who are at increased risk for severe, life-threatening myelosuppression from azathioprine. Death associated with pancytopenia has been reported in patients with absent TPMT activity receiving azathioprine.6, 20
Gastrointestinal
Nausea and vomiting may occur within the first few months of therapy with azathioprine, and occurred in approximately 12% of 676 rheumatoid arthritis patients. The frequency of gastric disturbance often can be reduced by administration of the drug in divided doses and/or after meals. However, in some patients, nausea and vomiting may be severe and may be accompanied by symptoms such as diarrhea, fever, malaise, and myalgias. Vomiting with abdominal pain may occur rarely with a hypersensitivity pancreatitis.
Hepatotoxicity manifest by elevation of serum alkaline phosphatase, bilirubin and/or serum transaminases is known to occur following azathioprine use, primarily in allograft recipients. Hepatotoxicity has been uncommon (less than 1%) in rheumatoid arthritis patients. Hepatotoxicity following transplantation most often occurs within 6 months of transplantation and is generally reversible after interruption of azathioprine. A rare, but life-threatening hepatic veno-occlusive disease associated with chronic administration of azathioprine has been described in transplant patients and in one patient receiving azathioprine for panuveitis.21,22,23 Periodic measurement of serum transaminases, alkaline phosphatase and bilirubin is indicated for early detection of hepatotoxicity. If hepatic veno-occlusive disease is clinically suspected, azathioprine should be permanently withdrawn.
Others
Additional side effects of low frequency have been reported. These include skin rashes, alopecia, fever, arthralgias, diarrhea, steatorrhea, negative nitrogen balance, reversible interstitial pneumonitis, hepatosplenic T-cell lymphoma.
OVERDOSAGE
The oral LD50s for single doses of azathioprine in mice and rats are 2500 mg/kg and 400 mg/kg, respectively. Very large doses of this antimetabolite may lead to marrow hypoplasia, bleeding, infection, and death. About 30% of azathioprine is bound to serum proteins, but approximately 45% is removed during an 8-hour hemodialysis.24 A single case has been reported of a renal transplant patient who ingested a single dose of 7500 mg azathioprine. The immediate toxic reactions were nausea, vomiting, and diarrhea, followed by mild leukopenia and mild abnormalities in liver function. The white blood cell count, SGOT, and bilirubin returned to normal 6 days after the overdose.
DOSAGE AND ADMINISTRATION
TPMT TESTING CANNOT SUBSTITUTE FOR COMPLETE BLOOD COUNT (CBC) MONITORING IN PATIENTS RECEIVING AZATHIOPRINE. TPMT genotyping or phenotyping can be used to identify patients with absent or reduced TPMT activity. Patients with low or absent TPMT activity are at an increased risk of developing severe, life-threatening myelotoxicity from azathioprine if conventional doses are given. Physicians may consider alternative therapies for patients who have low or absent TPMT activity (homozygous for non-functional alleles). Azathioprine should be administered with caution to patients having one non-functional allele (heterozygous) who are at risk for reduced TPMT activity that may lead to toxicity if conventional doses are given. Dosage reduction is recommended in patients with reduced TPMT activity. Early drug discontinuation may be considered in patients with abnormal CBC results that do not respond to dose reduction.
Renal Homotransplantation
The dose of azathioprine required to prevent rejection and minimize toxicity will vary with individual patients; this necessitates careful management. The initial dose is usually 3 to 5 mg/kg daily, beginning at the time of transplant. Azathioprine is usually given as a single daily dose on the day of, and in a minority of cases 1 to 3 days before, transplantation. Azathioprine is often initiated with the intravenous administration of the sodium salt, with subsequent use of tablets (at the same dose level) after the postoperative period. Intravenous administration of the sodium salt is indicated only in patients unable to tolerate oral medications. Dose reduction to maintenance levels of 1 to 3 mg/kg daily is usually possible. The dose of azathioprine should not be increased to toxic levels because of threatened rejection. Discontinuation may be necessary for severe hematologic or other toxicity, even if rejection of the homograft may be a consequence of drug withdrawal.
Rheumatoid Arthritis
Azathioprine is usually given on a daily basis. The initial dose should be approximately 1 mg/kg (50 to 100 mg) given as a single dose or on a twice-daily schedule. The dose may be increased, beginning at 6 to 8 weeks and thereafter by steps at 4-week intervals, if there are no serious toxicities and if initial response is unsatisfactory. Dose increments should be 0.5 mg/kg daily, up to a maximum dose of 2.5 mg/kg/day. Therapeutic response occurs after several weeks of treatment, usually 6 to 8; an adequate trial should be a minimum of 12 weeks. Patients not improved after 12 weeks can be considered refractory. Azathioprine may be continued long-term in patients with clinical response, but patients should be monitored carefully, and gradual dosage reduction should be attempted to reduce risk of toxicities.
Maintenance therapy should be at the lowest effective dose, and the dose given can be lowered decrementally with changes of 0.5 mg/kg or approximately 25 mg daily every 4 weeks while other therapy is kept constant. The optimum duration of maintenance azathioprine has not been determined. Azathioprine can be discontinued abruptly, but delayed effects are possible.
Use in Renal Dysfunction
Relatively oliguric patients, especially those with tubular necrosis in the immediate postcadaveric transplant period, may have delayed clearance of azathioprine or its metabolites, may be particularly sensitive to this drug, and are usually given lower doses.
Parenteral Administration
Add 10 mL of Sterile Water for Injection, and swirl until a clear solution results. This solution, equivalent to 100 mg azathioprine, is for intravenous use only; it has a pH of approximately 9.6, and it should be used within 24 hours. Further dilution into sterile saline or dextrose is usually made for infusion; the final volume depends on time for the
infusion, usually 30 to 60 minutes, but as short as 5 minutes and as long as 8 hours for the daily dose.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Procedures for proper handling and disposal of this immunosuppressive antimetabolite drug should be considered. Several guidelines on this subject have been published.25-31 There is no general agreement that all of the procedures recommended in the guidelines are necessary or appropriate.
HOW SUPPLIED
Azathioprine Sodium for Injection, USP, is supplied in a 20 mL vial, each containing azathioprine sodium, equivalent to 100 mg azathioprine.
Store at 20° to 25°C (68° to 77°F).
Protect from light. Retain in carton until time of use.
The sterile, lyophilized sodium salt is yellow, and should be dissolved in Sterile Water for Injection
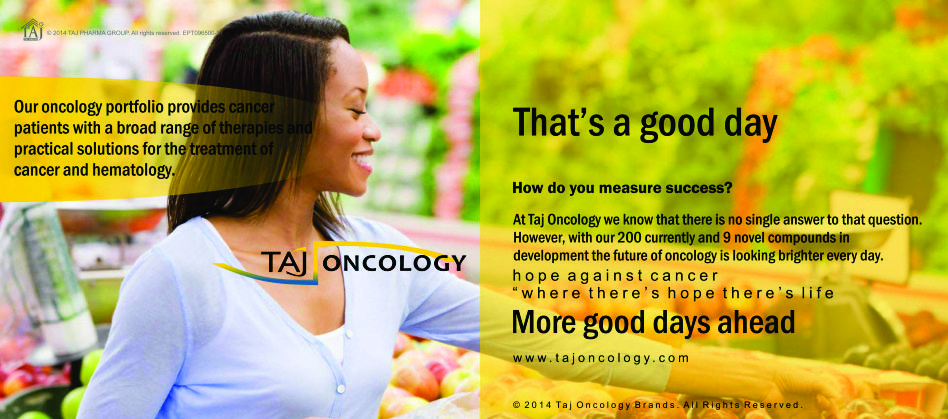
Product Glimpse
Description
We are committed to work towards a healthier and happier world. The company is an integrated, research based international pharmaceutical company, producing a wide range of quality, affordable generic (Azathioprine Sodium 100mg Injection) medicines, trusted by health-care professionals and patients across geographies.
We offer you the highest quality new Generic medicines ie. Azathioprine Sodium 100mg Injection, drugs and also with innovative packing at the lowest prices shipped to you from India. Browse our latest Pharmaceuticals and Generics possibilities and other pharmaceuticals possibilities…more.