Mitotane 500mg Tablets
Mitotane
Mitotane 500mg Tablets
Mitotane is a white granular solid composed of clear colorless crystals. It is tasteless and has a slight pleasant aromatic odor. It is soluble in ethanol, isooctane, and carbon tetrachloride. It has a molecular weight of 320.05.
Inactive ingredients in Mitotane tablets are: avicel, Polyethylene Glycol 3350, silicon dioxide, and starch.
Mitotane is available as 500 mg scored tablets for oral administration.
Mitotane should be administered under the supervision of a qualified physician experienced in the uses of cancer chemotherapeutic agents. Mitotane should be temporarily discontinued immediately following shock or severe trauma since adrenal suppression is its prime action. Exogenous steroids should be administered in such circumstances, since the depressed adrenal may not immediately start to secrete steroids.
Mitotane Tablets, USP
500 mg Tablets, bottle of 100
Store at 25°C (77°F); excursions permitted to 15°C-30°C (59°F-86°F) [see USP Controlled Room Temperature].
Mitotane
Mitotane 500mg Tablets
What Mitotane is and what it is used for
Mitotane is an antitumoral medicine.
This medicine is used for the treatment of symptoms of advanced non operable, metastatic or recurrent malignant tumours of the adrenal glands.
What you need to know before you take Mitotane
Do not take Mitotane
- if you are allergic to mitotane or any of the other ingredients of this medicine (listed in section 6).
- if you are breast-feeding. You must not breast-feed while taking Mitotane.
- if you are being treated with medicines containing spironolactone (see "Other medicines and Mitotane").
Warnings and precautions
Talk to your doctor or pharmacist before taking Mitotane.
You should tell your doctor if any of the following applies to you:
- if you have an injury (shock, severe trauma), an infection or if you have any illness while you are taking Mitotane. Tell your doctor immediately, who may decide to temporarily stop treatment.
- if you have severe liver or kidney problems.
- if you are using any medicines mentioned below (see "Other medicines and Mitotane").
This medicine should not be handled by persons other than the patient and his/her caregivers, and especially not by pregnant women. Caregivers should wear disposable gloves when handling the tablets.
Your doctor may prescribe you some hormonal treatment (steroids) while you are taking Mitotane.
Always keep with you the Mitotane Patient Card included at the end of this leaflet.
Other medicines and Mitotane
Please tell your doctor or pharmacist if you are using or have recently used any other medicines, including medicines obtained without a prescription.
You must not use Mitotane with medicines containing spironolactone, often used as a diuretic for heart, liver or kidney diseases.
Mitotane may interfere with several medicines. Therefore, you should tell your doctor if you are using medicines containing any of the following active substances:
- warfarin or other anticoagulants (blood thinners), used to prevent blood clots. The dose of your anticoagulant may need adjustment.
- antiepileptics
- rifabutin or rifampicin, used to treat tuberculosis
- griseofulvin, used in the treatment of fungal infections
- herbal preparations containing St. John’s wort (Hypericum perforatum)
Mitotane with food and drink
Mitotane should preferably be taken during meals containing fat-rich food such as milk, chocolate, oil.
Pregnancy, breast-feeding and fertility
Mitotane may harm the foetus. If you are pregnant or planning to become pregnant, tell your doctor.
If you may become pregnant, you should use effective contraception during treatment with Mitotane and even after stopping it. Ask your doctor for advice.
You must not breast-feed while taking Mitotane and even after stopping it. Ask your doctor for advice.
Driving and using machines
Mitotane has a major influence on your ability to drive and use machines. Ask your doctor for advice.
How to take Mitotane
Always take this medicine exactly as your doctor has told you. Check with your doctor or pharmacist if you are not sure.
Dose and schedule
The usual starting dose for adults is 2 to 3 g (4 to 6 tablets) per day.
Your doctor may start treatment at higher doses such as 4 to 6 g (8 to 12 tablets).
In order to find the optimal dose for you, your doctor will monitor regularly the levels of Mitotane in your blood. Your doctor may decide to stop treatment with Mitotane temporarily or to lower the dose if you experience certain side effects.
Use in children and adolescents The starting daily dose of Mitotane is 1.5 to 3.5 g/m2 body surface (this will be calculated by your doctor according to the weight and the size of the child). The experience in patients in this age group is very limited.
Method of administration
You should swallow the tablets with a glass of water during meals containing fat-rich food. You can divide the total daily dose in two or three intakes.
If you take more Mitotane than you should
Tell your doctor immediately if you have taken accidentally more Mitotane than you should or if a child has accidentally swallowed some.
If you forget to take Mitotane
If you accidentally miss a dose, just take the next dose as scheduled. Do not take a double dose to make up for the forgotten one.
If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
Possible side effects
Like all medicines, Mitotane can cause side effects, although not everybody gets them.
Tell your doctor immediately if you experience any of the following side effects:
- Adrenal insufficiency: fatigue, abdominal pain, nausea, vomiting, diarrhoea, confusion
- Anaemia: cutaneous pallor, muscular fatigability, feeling breathless, vertigo especially when standing up
- Liver damage: yellowing of the skin and eyes, itching, nausea, diarrhoea, fatigue, dark coloured urine
- Neurological disorders: movement and coordination disorders, abnormal sensations like pins and needles, memory loss, concentration difficulty, difficulty to talk, vertigo
These symptoms may reveal complications for which specific medication could be appropriate.
Side effects may occur with certain frequencies, which are defined as follows:
- very common: may affect more than 1 in 10 people
- common: may affect up to 1 in 10 people
- not known: frequency cannot be estimated from the available data
Very common side effects
- vomiting, nausea (feeling sick), diarrhoea, belly pain
- lack of appetite
- abnormal sensations like pins and needles
- movement and coordination disorders, vertigo, confusion
- feeling sleepy, fatigue, muscle weakness (fatigue of muscle during effort)
- inflammation (swelling, heat, pain) of mucosa, skin rash
- blood disorders (bleeding time prolonged)
- increase of cholesterol, triglycerides (fats) and liver enzymes (in blood tests)
- decrease in white blood cells count
- breast overdevelopment in men
- adrenal insufficiency
Common side effects
- dizziness, headache
- peripheral nervous system disorders (association of sensory disorders, muscular weakness and atrophy, decrease of tendon reflex and vasomotor symptoms such as hot flushes, sweat and sleep disorders)
- mental impairment (such as memory loss, concentration difficulty)
- movement disorder
- decrease of red blood cells (anaemia, with symptoms such as skin pallor and fatigue), decrease in blood platelets (may make you more prone to bruising and bleeding)
- hepatitis (auto-immune) (may cause yellowing of the skin and eyes, dark coloured urine)
- difficulty of coordinating muscles
Frequency Not Known
- fever
- general aching
- flushing, high or low blood pressure, feeling of dizziness/vertigo when you suddenly stand up
- increased production of saliva
- eye disorders: visual impairment, vision blurred, double vision, distortion of images, complain of glare
- fungal infection
- liver damage (may cause yellowing of the skin and eyes, dark coloured urine)
- decreased uric acid in blood tests
- bladder inflammation with bleeding
- presence of blood in urine, presence of proteins in urine
- balance disorder
- distortion of the sense of taste
- impaired indigestion
In children and adolescents, thyroid problems, neuro-psychological, growth retardation and one case of encephalopathy have been observed.
Reporting of side effects
If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the national reporting system listed in Appendix V. By reporting side effects you can help provide more information on the safety of the medicine.
How to store Mitotane
Keep out of the sight and reach of children.
Store in the original packaging.
Do not use after the expiry date which is stated on the carton and the bottle after EXP.
Any unused product or waste material should be disposed of in accordance with local requirements for cytotoxic medicines.
Do not throw away any medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. These measures will help protect the environment.
Contents of the pack and other information
What Mitotane contains
The active substance is mitotane. Each tablet contains 500 mg of mitotane.
The other ingredients are maize starch, microcrystalline cellulose (E 460), macrogol 3350 and silica colloidal anhydrous.
What Mitotane looks like and contents of the pack
Mitotane tablets are white, biconvex, round and scored. Mitotane is available in plastic bottles of 100 tablets.
Mitotane
Mitotane 500mg Tablets
DESCRIPTION
Mitotane Tablets is an oral chemotherapeutic agent. It is best known by its trivial name, o,p′-DDD, and is chemically, 1,1-dichloro-2-(o-chlorophenyl)-2-(p-chlorophenyl) ethane. The chemical structure is shown below:

Mitotane is a white granular solid composed of clear colorless crystals. It is tasteless and has a slight pleasant aromatic odor. It is soluble in ethanol, isooctane, and carbon tetrachloride. It has a molecular weight of 320.05.
Inactive ingredients in Mitotane tablets are: avicel, Polyethylene Glycol 3350, silicon dioxide, and starch.
Mitotane is available as 500 mg scored tablets for oral administration.
CLINICAL PHARMACOLOGY
Mitotane can best be described as an adrenal cytotoxic agent, although it can cause adrenal inhibition, apparently without cellular destruction. Its biochemical mechanism of action is unknown. Data are available to suggest that the drug modifies the peripheral metabolism of steroids as well as directly suppressing the adrenal cortex. The administration of Mitotane alters the extra-adrenal metabolism of cortisol in man; leading to a reduction in measurable 17-hydroxy corticosteroids, even though plasma levels of corticosteroids do not fall. The drug apparently causes increased formation of 6-β-hydroxycortisol.
Data in adrenal carcinoma patients indicate that about 40% of oral Mitotane is absorbed and approximately 10% of the administered dose is recovered in the urine as a water-soluble metabolite. A variable amount of metabolite (1%-17%) is excreted in the bile and the balance is apparently stored in the tissues.
Following discontinuation of Mitotane, the plasma terminal half-life has ranged from 18 to 159 days. In most patients blood levels become undetectable after 6 to 9 weeks. Autopsy data have provided evidence that Mitotane is found in most tissues of the body; however, fat tissues are the primary site of storage. Mitotane is converted to a water-soluble metabolite.
No unchanged Mitotane has been found in urine or bile.
INDICATIONS AND USAGE
Mitotane is indicated in the treatment of inoperable adrenal cortical carcinoma of both functional and nonfunctional types.
CONTRAINDICATIONS
Mitotane should not be given to individuals who have demonstrated a previous hypersensitivity to it.
WARNINGS
Mitotane should be temporarily discontinued immediately following shock or severe trauma, since adrenal suppression is its prime action. Exogenous steroids should be administered in such circumstances, since the depressed adrenal may not immediately start to secrete steroids.
Mitotane should be administered with care to patients with liver disease other than metastatic lesions from the adrenal cortex, since the metabolism of Mitotane may be interfered with and the drug may accumulate.
All possible tumor tissues should be surgically removed from large metastatic masses before Mitotane administration is instituted. This is necessary to minimize the possibility of infarction and hemorrhage in the tumor due to a rapid cytotoxic effect of the drug.
Long-term continuous administration of high doses of Mitotane may lead to brain damage and impairment of function. Behavioral and neurological assessments should be made at regular intervals, since toxicity may be reversible after discontinuation of Mitotane. Literature reports suggest that mitotane plasma concentrations exceeding 20 mcg/mL are associated with a greater incidence of high grade central nervous system toxicity.
A substantial percentage of the patients treated show signs of adrenal insufficiency. It therefore appears necessary to watch for and institute steroid replacement in those patients. However, some investigators have recommended that steroid replacement therapy be administered concomitantly with Mitotane. It has been shown that the metabolism of exogenous steroids is modified and consequently somewhat higher doses than normal replacement therapy may be required. Since Mitotane increases hormone binding proteins, measurement of free cortisol and corticotropin (ACTH) levels may be useful in achieving optimal steroid replacement.
PRECAUTIONS
General
Adrenal insufficiency may develop in patients treated with Mitotane, and adrenal steroid replacement should be considered for these patients.
Since sedation, lethargy, vertigo, and other CNS side effects can occur, ambulatory patients should be cautioned about driving, operating machinery, and other hazardous pursuits requiring mental and physical alertness.
Prolonged bleeding time has been reported in patients treated with Mitotane. Consider this possibility prior to any surgical intervention.
Drug Interactions
Mitotane is a strong inducer of cytochrome P-450 3A4 (CYP3A4). Monitor patients for a change in dosage requirements for the concomitant drug when administering Mitotane to patients receiving drugs that are substrates of CYP3A4.
Mitotane’s CYP induction effect leads to an increase in dosage requirements for warfarin. Closely monitor patients for a change in anticoagulant dosage requirements when administering Mitotane to patients receiving coumarin-type anticoagulants.
Carcinogenesis, Mutagenesis, Impairment of Fertility
The carcinogenic and mutagenic potentials of Mitotane (mitotane tablets, USP) are unknown. However, the mechanism of action of this compound suggests that it probably has less carcinogenic potential than other cytotoxic chemotherapeutic drugs.
Pregnancy
Pregnancy Category D
Mitotane can cause fetal harm when administered to a pregnant woman. Abnormal pregnancy outcomes such as preterm births and early pregnancy loss have been reported in patients exposed to mitotane during pregnancy. Animal reproduction studies have not been conducted with Mitotane. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus.
Advise women of childbearing potential to use effective contraception during treatment and after discontinuation of treatment for as long as mitotane plasma levels are detectable.
Nursing Mothers
Mitotane has been detected in breast milk. Because of the potential for serious adverse reactions in nursing infants from mitotane, advise women to discontinue nursing during Mitotane therapy and after treatment discontinuation for as long as mitotane plasma levels are detectable.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
Geriatric Use
Clinical studies of Mitotane did not include sufficient numbers of patients aged 65 years and older to determine whether they respond differently than younger patients. Other reported clinical experience has not identified differences in responses between elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
ADVERSE REACTIONS
A very high percentage of patients treated with Mitotane have shown at least one type of side effect. The main types of adverse reactions consist of the following:
- Gastrointestinal disturbances, which consist of anorexia, nausea or vomiting, and in some cases diarrhea, occur in about 80% of the patients.
- Central nervous system side effects occur in 40% of the patients. These consist primarily of depression as manifested by lethargy and somnolence (25%), and dizziness or vertigo (15%).
- Skin toxicity has been observed in about 15% of the cases. These skin changes consist primarily of transient skin rashes which do not seem to be dose related. In some instances, this side effect subsided while the patients were maintained on the drug without a change of dose.
Infrequently occurring side effects involve the eye (visual blurring, diplopia, lens opacity, toxic retinopathy); the genitourinary system (hematuria, hemorrhagic cystitis, and albuminuria); cardiovascular system (hypertension, orthostatic hypotension, and flushing); and some miscellaneous effects including generalized aching, hyperpyrexia, and lowered protein bound iodine (PBI).
The following additional adverse reactions have been identified during postapproval use of Mitotane. Because reports are voluntary from a population of unknown size, an estimate of frequency cannot be made.
Blood and lymphatic system disorders:
neutropenia
Endocrine disorders:
growth retardation, hypothyroidism
Psychiatric disorders:
confusional state
Nervous system disorders:
neuropsychological disturbance, dysarthria, headache, ataxia, mental impairment
Eye disorders:
maculopathy
Hepatobiliary disorders:
hepatitis, elevation of liver enzymes
Reproductive system and breast disorders:
gynecomastia
General disorders and administration site conditions:
asthenia
Investigations:
blood uric acid decreased, blood cholesterol increased, blood triglycerides increased
OVERDOSAGE
No proven antidotes have been established for Mitotane overdosage. The long half-life of mitotane will require prolonged observation for toxicity.
DOSAGE AND ADMINISTRATION
The recommended treatment schedule is to start the patient at 2 g to 6 g of Mitotane per day in divided doses, either 3 or 4 times a day. Doses are usually increased incrementally to 9 g to 10 g per day. If severe side effects appear, the dose should be reduced until the maximum tolerated dose is achieved. If the patient can tolerate higher doses and improved clinical response appears possible, the dose should be increased until adverse reactions interfere. Experience has shown that the maximum tolerated dose (MTD) will vary from 2 g to 16 g per day, but has usually been 9 g to 10 g per day. The highest doses used in the studies to date were 18 g to 19 g per day.
Treatment should be instituted in the hospital until a stable dosage regimen is achieved.
Treatment should be continued as long as clinical benefits are observed. Maintenance of clinical status or slowing of growth of metastatic lesions can be considered clinical benefits if they can clearly be shown to have occurred.
If no clinical benefits are observed after 3 months at the maximum tolerated dose, the case would generally be considered a clinical failure. However, 10% of the patients who showed a measurable response required more than 3 months at the MTD. Early diagnosis and prompt institution of treatment improve the probability of a positive clinical response. Clinical effectiveness can be shown by reduction in tumor mass; reduction in pain, weakness or anorexia; and reduction of symptoms and signs due to excessive steroid production.
A number of patients have been treated intermittently with treatment being restarted when severe symptoms have reappeared. Patients often do not respond after the third or fourth such course. Experience accumulated to date suggests that continuous treatment with the maximum possible dosage of Mitotane is the best approach.
Procedures for proper handling and disposal of anticancer drugs should be considered. Several guidelines on this subject have been published.1
To minimize the risk of dermal exposure, always wear impervious gloves when handling bottles containing Mitotane tablets. Mitotane tablets should not be crushed. Personnel should avoid exposure to crushed and/or broken tablets. If contact with broken tablets occurs, wash immediately and thoroughly. More information is available in the references listed below.
HOW SUPPLIED
Mitotane (mitotane tablets, USP)
500 mg Tablets, bottle of 100
STORAGE
Store at 25°C (77°F); excursions permitted to 15°C-30°C (59°F-86°F) [see USP Controlled Room Temperature].
REFERENCES
- 1.
- OSHA. http://www.osha.gov/SLTC/hazardousdrugs/index.html
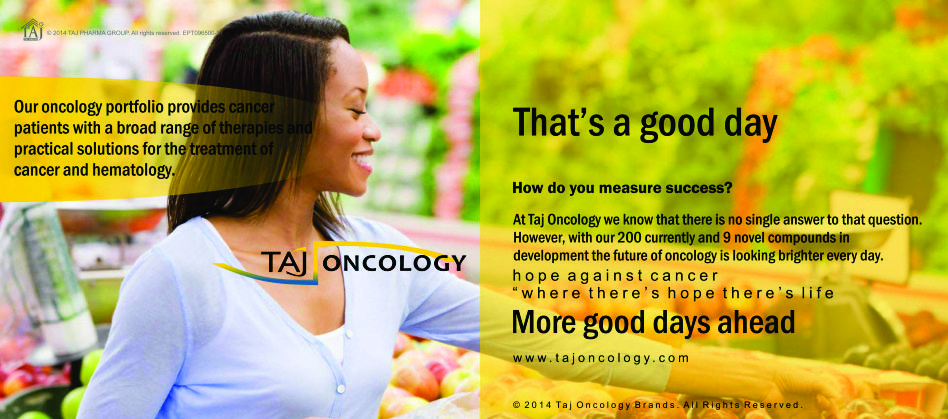
Product Glimpse
Description
We are committed to work towards a healthier and happier world. The company is an integrated, research based international pharmaceutical company, producing a wide range of quality, affordable generic (Mitotane 500mg Tablets) medicines, trusted by health-care professionals and patients across geographies.
We offer you the highest quality new Generic medicines ie. Mitotane 500mg Tablets, drugs and also with innovative packing at the lowest prices shipped to you from India. Browse our latest Pharmaceuticals and Generics possibilities and other pharmaceuticals possibilities…more.