Chlorambucil 1mg/2mg & 5mg Tablets
Chlorambucil
2mg Tablets
Chlorambucil is supplied as brown, film-coated, round, biconvex tablets containing 2 mg chlorambucil in amber glass bottles with child-resistant closures. One side is engraved with “GX EG3” and the other side is engraved with an “L.”
Bottle of 50.
Store in a refrigerator, 2° to 8°C (36° to 46°F).
Chlorambucil is indicated in the treatment of chronic lymphatic (lymphocytic) leukemia, malignant lymphomas including lymphosarcoma, giant follicular lymphoma, and Hodgkin’s disease. It is not curative in any of these disorders but may produce clinically useful palliation.
Ingredient contains:Aactive ingredient is chlorambucil. Each Chlorambucil tablet contains 2 mg of chlorambucil.
Other ingredients are microcrystalline cellulose, anhydrous lactose, colloidal anhydrous silica, stearic acid, hypromellose, titanium dioxide (E171), synthetic yellow iron oxide (E172), synthetic red iron oxide (E172) and macrogol.
Chlorambucil
2mg Tablets
What Chlorambucil is and What It Is Used For
The Tablets contains a medicine called chlorambucil. This belongs to a group of medicines called cytotoxics (also called chemotherapy). Chlorambucil is used to treat some types of cancer and certain blood problems. It works by reducing the number of abnormal cells your body makes.
Chlorambucil is used for:- Hodgkin's disease and Non-Hodgkins Lymphoma. Together, these form a group of diseases called lymphomas. They are cancers formed from cells of the lymphatic system.
- Chronic lymphocytic leukaemia. A disease where the bone marrow produces a large number of abnormal white cells.
- Waldenstrom's macroglobulinaemia is a rare blood condition involving the release of an abnormal protein into the blood.
Ask your doctor if you would like more explanation about these diseases.
vvBefore you take Chlorambucil Do not take Chlorambucil if:You are allergic (hypersensitive) to chlorambucil or any of the other ingredients of Chlorambucil tablets (See section 6: Further information)
Do not take Chlorambucil if the above applies to you. If you are not sure, talk to your doctor or pharmacist before taking Chlorambucil.
Take special care with ChlorambucilBefore you take Chlorambucil, tell your doctor or pharmacist if:
- you have had radiotherapy or chemotherapy, now or recently
- you have a liver or kidney problems
- you have nephrotic syndrome (a kidney problem) or ever had a fit or convulsion. You may have an increased risk of fits when taking Chlorambucil.If you are not sure if any of the above apply to you, talk to your doctor, nurse or pharmacist before taking Chlorambucil.
Please tell your doctor or pharmacist if you are taking or have recently taken any other medicines, including medicines obtained without a prescription. This includes herbal medicines.
In particular, tell your doctor or pharmacist if you are taking or have recently taken any of the following:
Do not take Chlorambucil if you are planning to have a baby. This applies to both men and women. Chlorambucil can affect ovaries or sperm, which may cause infertility (inability to have a baby). Use a reliable form of contraception to avoid pregnancy if either you or your partner is taking Chlorambucil. Ask your doctor for advice.
Pregnancy and breast-feedingTreatment with Chlorambucil is not recommended during pregnancy because it may cause permanent damage to a foetus. If you are pregnant, if you think you could be pregnant, or if you are planning to become pregnant, check with your doctor before you take Chlorambucil. Your doctor will consider the risks and benefits to you and your baby of taking Chlorambucil.
Do not breast-feed while taking Chlorambucil. There have been reports indicating that Chlorambucil and its ingredients can be passed into breast-milk. Ask your doctor or midwife for advice.
Important information about some of the ingredients of ChlorambucilChlorambucil tablets contain lactose. If you have been told by your doctor that you have an intolerance to some sugars, contact your doctor before you take Chlorambucil tablets.
How to take Chlorambucil
Chlorambucil should only be given to you by a specialist doctor who is experienced in treating cancer.
Always take Chlorambucil exactly as your doctor has told you. It is important to take your medicine at the right times. The label on your pack will tell you how many tablets to take and how often to take them. If the label doesn’t say or if you are not sure, ask your doctor, nurse or pharmacist.
- Chlorambucil is administrated orally and should be taken daily on an empty stomach (at least one hour before meals or three hours after meals).
- Swallow your tablets whole with a glass of water.
- Do not break, crush or chew the tablets.
The dose of Chlorambucil depends on your blood problem or cancer (see section 1).
Your doctor may change your dose during your treatment depending on your needs. The dose can sometimes be changed if you are elderly or have a kidney or liver problems.
When you take Chlorambucil your doctor will take regular blood tests. This is to check the number of cells in your blood. Your doctor may sometimes change your dose as a result.
The usual dose is 0.2 mg per kilogram of your body weight each day for adults and children.
Non-Hodgkin’s LymphomaThe usual dose is 0.1 to 0.2 mg per kilogram of your body weight each day for adults and children.
Chronic Lymphocytic LeukaemiaThe usual starting dose is 0.15 mg per kilogram of your body weight each day.
Waldenstrom's macroglobulinaemiaThe usual starting dose is 6 to 12 mg each day. Some people have to take Chlorambucil long term. If you have to take it long term, the usual dose is 2 to 8 mg each day. Follow your doctor’s instructions carefully.
If you take more Chlorambucil than you shouldIf you take more Chlorambucil than you should, tell your doctor immediately or go to a hospital straight away. Take the medicine pack with you.
If you forget to take ChlorambucilTell your doctor. Do not take a double dose to make up for a forgotten dose.
Possible Side Effects
Like all medicines, Chlorambucil can cause side effects, although not everybody gets them.
If you get any of the following, talk to your specialist doctor or go to hospital straight away:
- any signs of fever or infection (sore throat, sore mouth or urinary problems),
- any unexpected bruising or bleeding, as this could mean that too few blood cells of a particular type are being produced,
- if you suddenly feel unwell (even with a normal temperature),
- if you start feeling extremely tired,
- if you notice numbness or weakness of your muscles,
- if you experience skin rashes, blisters on the skin, sore mouth or eyes and have a high temperature.
Talk to your doctor if you have any of the following side effects, which may also happen with this medicine:
Very Common (affects more than 1 in 10 people)- a drop in the number of blood cells and platelets
- feeling sick (nausea), being sick (vomiting), diarrhoea or mouth ulcers
- secondary blood cancers (acute secondary haematologic malignancies)
- fits in children with a kidney problem known as nephrotic syndrome.
- a drop on red blood cells which may make you tired weak or breathless – called anaemia
- rash
- yellowing of the whites of the eyes or skin (jaundice)
- allergy symptoms such as skin lumps, hives or swelling of the tissues (oedema)
- on rare occasions, skin rash has been reported to progress to serious conditions including Stevens-Johnson syndrome and toxic epidermal necrolysis. These two forms of the same serious skin disease cause rash, skin peeling and stores on the mucous membranes.
- fever
- fit or convulsion. Patients are more at risk of having fits or convulsions if they have epilepsy and/or if they are being prescribed high doses
- abnormal and repetitive shaking movement of the body or twitching, without fits or convulsions
- inflammation of the bladder called cystitis
- irreversible bone marrow failure – your body may stop producing blood cells
- scarring and thickening in the lungs with shortness of breath
- lung disease
If any of the side effects get serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist.
It is possible that the use of Chlorambucil, particularly long term use, may increase the risk of developing a secondary blood cancer. In many cases, patients who develop this have also received another type of chemotherapy or some form of radiation therapy. Symptoms of a secondary haematological malignancy include tiredness, fever, infection and bruising. These side effects may also show up in your blood tests.
Tell your doctor as soon as possible if you have any of these symptoms. You may need to stop taking Chlorambucil, but only your doctor can tell you if that is the case.
How to store Chlorambucil
Keep out of the reach and sight of children.
Do not use Chlorambucil after the expiry date which is stated on the pack after ‘Exp’.
Store in a refrigerator between 2 and 8°C.
If your doctor tells you to stop taking the tablets, it is important to return any which are left over to your pharmacist, who will destroy them according to disposal of dangerous substance guidelines. Only keep the tablets if your doctor tells you to.
Further information
What Chlorambucil containsThe active ingredient is chlorambucil. Each Chlorambucil tablet contains 2 mg of chlorambucil.
The other ingredients are microcrystalline cellulose, anhydrous lactose, colloidal anhydrous silica, stearic acid, hypromellose, titanium dioxide (E171), synthetic yellow iron oxide (E172), synthetic red iron oxide (E172) and macrogol.
Chlorambucil tablets are brown, film-coated, round, biconvex tablets engraved ‘2’ on one side and ‘T’ on the other.
Chlorambucil tablets are in bottles of 25 tablets.
Chlorambucil
2mg Tablets
DESCRIPTION
Chlorambucil was first synthesized by Everett et al. It is a bifunctional alkylating agent of the nitrogen mustard type that has been found active against selected human neoplastic diseases. Chlorambucil is known chemically as 4-[bis(2-chlorethyl)amino]benzenebutanoic acid and has the following structural formula:

Chlorambucil hydrolyzes in water and has a pKa of 5.8.
Chlorambucil (chlorambucil) is available in tablet form for oral administration. Each film-coated tablet contains 2 mg chlorambucil and the inactive ingredients colloidal silicon dioxide, hypromellose, lactose (anhydrous), macrogol/PEG 400, microcrystalline cellulose, red iron oxide, stearic acid, titanium dioxide, and yellow iron oxide.
CLINICAL PHARMACOLOGY
Mechanism of ActionChlorambucil, an aromatic nitrogen mustard derivative, is an alkylating agent. Chlorambucil interferes with DNA replication and induces cellular apoptosis via the accumulation of cytosolic p53 and subsequent activation of Bax, an apoptosis promoter.
PharmacokineticsIn a study of 12 patients given single oral doses of 0.2 mg/kg of Chlorambucil, the mean dose-adjusted (±SD) plasma chlorambucil Cmax was 492 ± 160 ng/mL, the AUC was 883 ± 329 ng.h/mL, the mean elimination half-life (t½) was 1.3 ± 0.5 hours, and the Tmax was 0.83 ± 0.53 hours. For the major metabolite, phenylacetic acid mustard (PAAM), the mean dose-adjusted (± SD) plasma Cmax was 306 ± 73 ng/mL, the AUC was 1204 ± 285 ng.h/mL, mean t½ was 1.8 ± 0.4 hours, and the Tmax was 1.9 ± 0.7 hours.
After single oral doses of 0.6 to 1.2 mg/kg, peak plasma chlorambucil levels (Cmax) are reached within 1 hour and the terminal elimination half-life (t½) of the parent drug is estimated at 1.5 hours.
Absorption: Chlorambucil is rapidly and completely (>70%) absorbed from the gastrointestinal tract. Consistent with the rapid, predictable absorption of chlorambucil, the inter-individual variability in the plasma pharmacokinetics of chlorambucil has been shown to be relatively small following oral dosages of between 15 and 70 mg (2-fold intra-patient variability, and a 2 to 4 fold interpatient variability in AUC). The absorption of chlorambucil is reduced when taken after food. In a study of ten patients, food intake increased the median Tmax by 2-fold and reduced the dose-adjusted Cmax and AUC values by 55% and 20%, respectively.
Distribution: The apparent volume of distribution averaged 0.31 L/kg following a single 0.2 mg/kg oral dose of chlorambucil in 11 cancer patients with chronic lymphocytic leukemia.
Chlorambucil and its metabolites are extensively bound to plasma and tissue proteins. In vitro, chlorambucil is 99% bound to plasma proteins, specifically albumin. Cerebrospinal fluid levels of chlorambucil have not been determined.
Metabolism: Chlorambucil is extensively metabolized in the liver primarily to phenylacetic acid mustard, which has antineoplastic activity. Chlorambucil and its major metabolite undergo oxidative degradation to monohydroxy and dihydroxy derivatives.
Excretion: After a single dose of radiolabeled chlorambucil (14C), approximately 20% to 60% of the radioactivity appears in the urine after 24 hours. Again, less than 1% of the urinary radioactivity is in the form of chlorambucil or phenylacetic acid mustard.
INDICATIONS AND USAGE
Chlorambucil (chlorambucil) is indicated in the treatment of chronic lymphatic (lymphocytic) leukemia, malignant lymphomas including lymphosarcoma, giant follicular lymphoma, and Hodgkin’s disease. It is not curative in any of these disorders but may produce clinically useful palliation.
CONTRAINDICATIONS
Chlorambucil should not be used in patients whose disease has demonstrated a prior resistance to the agent. Patients who have demonstrated hypersensitivity to chlorambucil should not be given the drug. There may be cross-hypersensitivity (skin rash) between chlorambucil and other alkylating agents.
WARNINGS
Because of its carcinogenic properties, chlorambucil should not be given to patients with conditions other than chronic lymphatic leukemia or malignant lymphomas. Convulsions, infertility, leukemia, and secondary malignancies have been observed when chlorambucil was employed in the therapy of malignant and non-malignant diseases.
There are many reports of acute leukemia arising in patients with both malignant and non-malignant diseases following chlorambucil treatment. In many instances, these patients also received other chemotherapeutic agents or some form of radiation therapy. The quantitation of the risk of chlorambucil-induction of leukemia or carcinoma in humans is not possible. Evaluation of published reports of leukemia developing in patients who have received chlorambucil (and other alkylating agents) suggests that the risk of leukemogenesis increases with both chronicity of treatment and large cumulative doses. However, it has proved impossible to define a cumulative dose below which there is no risk of the induction of secondary malignancy. The potential benefits from chlorambucil therapy must be weighed on an individual basis against the possible risk of the induction of a secondary malignancy.
Chlorambucil has been shown to cause chromatid or chromosome damage in humans. Both reversible and permanent sterility have been observed in both sexes receiving chlorambucil.
A high incidence of sterility has been documented when chlorambucil is administered to prepubertal and pubertal males. Prolonged or permanent azoospermia has also been observed in adult males. While most reports of gonadal dysfunction secondary to chlorambucil have related to males, the induction of amenorrhea in females with alkylating agents is well documented and chlorambucil is capable of producing amenorrhea. Autopsy studies of the ovaries from women with malignant lymphoma treated with combination chemotherapy including chlorambucil have shown varying degrees of fibrosis, vasculitis, and depletion of primordial follicles.
.
Rare instances of skin rash progressing to erythema multiforme, toxic epidermal necrolysis, or Stevens-Johnson syndrome have been reported. Chlorambucil should be discontinued promptly in patients who develop skin reactions.
Pregnancy Category D. Chlorambucil can cause fetal harm when administered to a pregnant woman. Unilateral renal agenesis has been observed in 2 offspring whose mothers received chlorambucil during the first trimester. Urogenital malformations, including absence of a kidney, were found in fetuses of rats given chlorambucil. There are no adequate and well-controlled studies in pregnant women. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus. Women of childbearing potential should be advised to avoid becoming pregnant.
PRECAUTIONS
GeneralMany patients develop a slowly progressive lymphopenia during treatment. The lymphocyte count usually rapidly returns to normal levels upon completion of drug therapy. Most patients have some neutropenia after the third week of treatment and this may continue for up to 10 days after the last dose. Subsequently, the neutrophil count usually rapidly returns to normal. Severe neutropenia appears to be related to dosage and usually occurs only in patients who have received a total dosage of 6.5 mg/kg or more in one course of therapy with continuous dosing. About one quarter of all patients receiving the continuous-dose schedule, and one third of those receiving this dosage in 8 weeks or less may be expected to develop severe neutropenia.
While it is not necessary to discontinue chlorambucil at the first evidence of a fall in neutrophil count, it must be remembered that the fall may continue for 10 days after the last dose, and that as the total dose approaches 6.5 mg/kg, there is a risk of causing irreversible bone marrow damage. The dose of chlorambucil should be decreased if leukocyte or platelet counts fall below normal values and should be discontinued for more severe depression.
Chlorambucil should not be given at full dosages before 4 weeks after a full course of radiation therapy or chemotherapy because of the vulnerability of the bone marrow to damage under these conditions. If the pretherapy leukocyte or platelet counts are depressed from bone marrow disease process prior to institution of therapy, the treatment should be instituted at a reduced dosage.
Persistently low neutrophil and platelet counts or peripheral lymphocytosis suggest bone marrow infiltration. If confirmed by bone marrow examination, the daily dosage of chlorambucil should not exceed 0.1 mg/kg. Chlorambucil appears to be relatively free from gastrointestinal side effects or other evidence of toxicity apart from the bone marrow depressant action. In humans, single oral doses of 20 mg or more may produce nausea and vomiting.
Children with nephrotic syndrome and patients receiving high pulse doses of chlorambucil may have an increased risk of seizures. As with any potentially epileptogenic drug, caution should be exercised when administering chlorambucil to patients with a history of seizure disorder or head trauma, or who are receiving other potentially epileptogenic drugs.
Administration of live vaccines to immunocompromised patients should be avoided.
Patients should be informed that the major toxicities of chlorambucil are related to hypersensitivity, drug fever, myelosuppression, hepatotoxicity, infertility, seizures, gastrointestinal toxicity, and secondary malignancies. Patients should never be allowed to take the drug without medical supervision and should consult their physician if they experience skin rash, bleeding, fever, jaundice, persistent cough, seizures, nausea, vomiting, amenorrhea, or unusual lumps/masses. Women of childbearing potential should be advised to avoid becoming pregnant.
Laboratory TestsPatients must be followed carefully to avoid life-endangering damage to the bone marrow during treatment. Weekly examination of the blood should be made to determine hemoglobin levels, total and differential leukocyte counts, and quantitative platelet counts. Also, during the first 3 to 6 weeks of therapy, it is recommended that white blood cell counts be made 3 or 4 days after each of the weekly complete blood counts. Galton et al have suggested that in following patients it is helpful to plot the blood counts on a chart at the same time that body weight, temperature, spleen size, etc., are recorded. It is considered dangerous to allow a patient to go more than 2 weeks without hematological and clinical examination during treatment.
Drug InteractionsThere are no known drug/drug interactions with chlorambucil.
Carcinogenesis, Mutagenesis, Impairment of FertilitySee WARNINGS section for information on carcinogenesis, mutagenesis, and impairment of fertility.
PregnancyTeratogenic Effects: Pregnancy Category D: See WARNINGS section.
Nursing MothersIt is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from chlorambucil, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric UseThe safety and effectiveness in pediatric patients have not been established.
Geriatric UseClinical studies of chlorambucil did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Use in Patients with Renal Impairment: The impact of renal impairment on chlorambucil elimination has not been formally studied. The renal elimination of unchanged chlorambucil and its major active metabolites, phenylacetic acid mustard, represents less than 1% of the administered dose. In addition, no dose adjustment was required in 2 dialysis patients on chlorambucil. Therefore, renal impairment is not expected to significantly impact the elimination of chlorambucil.
Use in Patients with Hepatic Impairment: No formal studies have been conducted in patients with hepatic impairment. As chlorambucil is primarily metabolized in the liver, patients with hepatic impairment should be closely monitored for toxicity and dose reduction may be considered in patients with hepatic impairment when treated with Chlorambucil (see DOSAGE AND ADMINISTRATION).
ADVERSE REACTIONS
To report SUSPECTED ADVERSE REACTIONS, contact Aspen Global Inc. FDA or www.fda.gov/medwatch.
HematologicThe most common side effect is bone marrow suppression, anemia, leukopenia, neutropenia, thrombocytopenia, or pancytopenia. Although bone marrow suppression frequently occurs, it is usually reversible if the chlorambucil is withdrawn early enough. However, irreversible bone marrow failure has been reported.
GastrointestinalGastrointestinal disturbances such as nausea and vomiting, diarrhea, and oral ulceration occur infrequently.
CNSTremors, muscular twitching, myoclonia, confusion, agitation, ataxia, flaccid paresis, and hallucinations have been reported as rare adverse experiences to chlorambucil which resolve upon discontinuation of drug. Rare, focal and/or generalized seizures have been reported to occur in both children and adults at both therapeutic daily doses and pulse-dosing regimens, and in acute overdose (see PRECAUTIONS: General).
DermatologicAllergic reactions such as urticaria and angioneurotic edema have been reported following initial or subsequent dosing. Skin hypersensitivity (including rare reports of skin rash progressing to erythema multiforme, toxic epidermal necrolysis, and Stevens-Johnson syndrome) has been reported (see WARNINGS).
MiscellaneousOther reported adverse reactions include: pulmonary fibrosis, hepatotoxicity and jaundice, drug fever, peripheral neuropathy, interstitial pneumonia, sterile cystitis, infertility, leukemia, and secondary malignancies (see WARNINGS).
OVERDOSAGE
Reversible pancytopenia was the main finding of inadvertent overdoses of chlorambucil. Neurological toxicity ranging from agitated behavior and ataxia to multiple grand mal seizures has also occurred. As there is no known antidote, the blood picture should be closely monitored and general supportive measures should be instituted, together with appropriate blood transfusions, if necessary. Chlorambucil is not dialyzable.
Oral LD50 single doses in mice are 123 mg/kg. In rats, a single intraperitoneal dose of 12.5 mg/kg of chlorambucil produces typical nitrogen-mustard effects; these include atrophy of the intestinal mucous membrane and lymphoid tissues, severe lymphopenia becoming maximal in 4 days, anemia, and thrombocytopenia. After this dose, the animals begin to recover within 3 days and appear normal in about a week, although the bone marrow may not become completely normal for about 3 weeks. An intraperitoneal dose of 18.5 mg/kg kills about 50% of the rats with development of convulsions. As much as 50 mg/kg has been given orally to rats as a single dose, with recovery. Such a dose causes bradycardia, excessive salivation, hematuria, convulsions, and respiratory dysfunction.
DOSAGE AND ADMINISTRATION
The usual oral dosage is 0.1 to 0.2 mg/kg body weight daily for 3 to 6 weeks as required. This usually amounts to 4 to 10 mg per day for the average patient. The entire daily dose may be given at one time. These dosages are for initiation of therapy or for short courses of treatment. The dosage must be carefully adjusted according to the response of the patient and must be reduced as soon as there is an abrupt fall in the white blood cell count. Patients with Hodgkin’s disease usually require 0.2 mg/kg daily, whereas patients with other lymphomas or chronic lymphocytic leukemia usually require only 0.1 mg/kg daily. When lymphocytic infiltration of the bone marrow is present, or when the bone marrow is hypoplastic, the daily dose should not exceed 0.1 mg/kg (about 6 mg for the average patient).
Alternate schedules for the treatment of chronic lymphocytic leukemia employing intermittent, biweekly, or once-monthly pulse doses of chlorambucil have been reported. Intermittent schedules of chlorambucil begin with an initial single dose of 0.4 mg/kg. Doses are generally increased by 0.1 mg/kg until control of lymphocytosis or toxicity is observed. Subsequent doses are modified to produce mild hematologic toxicity. It is felt that the response rate of chronic lymphocytic leukemia to the biweekly or once-monthly schedule of chlorambucil administration is similar or better to that previously reported with daily administration and that hematologic toxicity was less than or equal to that encountered in studies using daily chlorambucil.
Radiation and cytotoxic drugs render the bone marrow more vulnerable to damage, and chlorambucil should be used with particular caution within 4 weeks of a full course of radiation therapy or chemotherapy. However, small doses of palliative radiation over isolated foci remote from the bone marrow will not usually depress the neutrophil and platelet count. In these cases chlorambucil may be given in the customary dosage.
It is presently felt that short courses of treatment are safer than continuous maintenance therapy, although both methods have been effective. It must be recognized that continuous therapy may give the appearance of “maintenance” in patients who are actually in remission and have no immediate need for further drug. If maintenance dosage is used, it should not exceed 0.1 mg/kg daily and may well be as low as 0.03 mg/kg daily. A typical maintenance dose is 2 mg to 4 mg daily, or less, depending on the status of the blood counts. It may, therefore, be desirable to withdraw the drug after maximal control has been achieved, since intermittent therapy reinstituted at time of relapse may be as effective as continuous treatment.
Procedures for proper handling and disposal of anticancer drugs should be used. Several guidelines on this subject have been published.1-4 There is no general agreement that all of the procedures recommended in the guidelines are necessary or appropriate.
Hepatic Impairment: Patients with hepatic impairment should be closely monitored for toxicity. As chlorambucil is primarily metabolized in the liver, dose reduction may be considered in patients with hepatic impairment when treated with Chlorambucil. However, there are insufficient data in patients with hepatic impairment to provide a specific dosing recommendation.
HOW SUPPLIED
Chlorambucil is supplied as brown, film-coated, round, biconvex tablets containing 2 mg chlorambucil in amber glass bottles with child-resistant closures. One side is engraved with “GX EG3” and the other side is engraved with an “L.”
Bottle of 50.
Store in a refrigerator, 2° to 8°C (36° to 46°F).
REFERENCES
1. NIOSH Alert: Preventing occupational exposures to antineoplastic and other hazardous drugs in healthcare settings. 2004. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 2004-165.
2. OSHA Technical Manual, TED 1-0.15A, Section VI: Chapter 2. Controlling Occupational Exposure to Hazardous Drugs. OSHA, 1999. http://www.osha.gov/dts/osta/otm/otm_vi/otm_vi_2.html
3. American Society of Health-System Pharmacists. ASHP guidelines on handling hazardous drugs. Am J Health-Syst Pharm. (2006) 63:1172-1193.
4. Polovich, M., White, J. M., & Kelleher, L.O. (eds.) 2005. Chemotherapy and biotherapy guidelines and recommendations for practice (2nd. ed.) Pittsburgh, PA: Oncology Nursing Society.
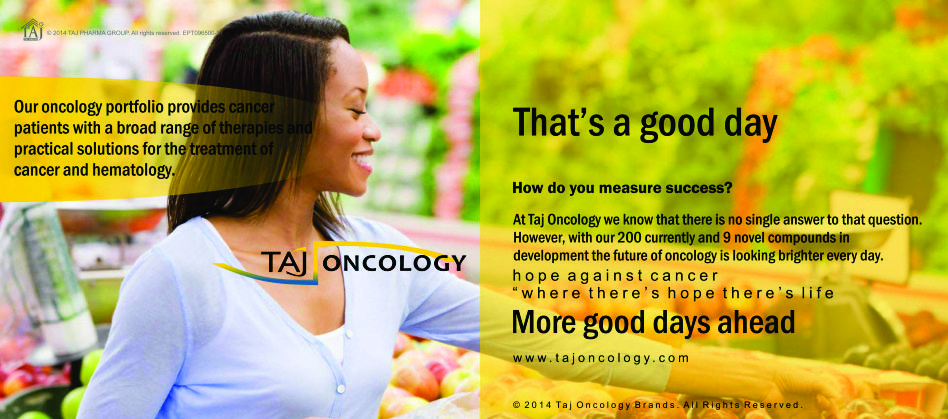
Product Glimpse
Description
We are committed to work towards a healthier and happier world. The company is an integrated, research based international pharmaceutical company, producing a wide range of quality, affordable generic (Chlorambucil 1mg/2mg & 5mg Tablets) medicines, trusted by health-care professionals and patients across geographies.
We offer you the highest quality new Generic medicines ie. Chlorambucil 1mg/2mg & 5mg Tablets, drugs and also with innovative packing at the lowest prices shipped to you from India. Browse our latest Pharmaceuticals and Generics possibilities and other pharmaceuticals possibilities…more.